Methods to prevent bleeding:
-
- Manual pressure
- Devices which apply pressure over puncture site
- Systems to seal the arterial puncture with a plug of collagen
If artery is punctured above inguinal ligament severe bruising may not be visible in the groin – it may track upwards, causing retroperitoneal bleeding and present with hypotension and shock.
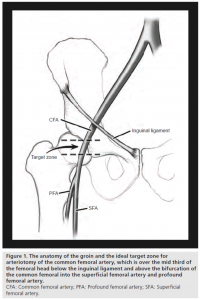
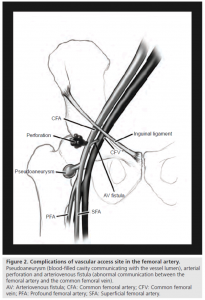
“Figure 1. The anatomy of the groin; Figure 2. Complications of the fermoral artery” Shaun Bhatty, Richard Cooke, Ranjith Shetty, Ion S Jovin and Mary Beatty-Brooks is licensed under CC BY 4.0
Monitoring to detect complications at the puncture site
Iain is monitored with frequent NEWS and NIHSS, in a similar way to patients who have had thrombolysis. However, the team need to be alert to some additional serious complications – in particular at the arterial puncture site, which is usually in the groin. This is even more likely in patients who have had thrombolysis or, like Iain, are taking oral anticoagulants.
Drag the words
Bleeding at the arterial puncture is the most common complication. The interventionalist will advise on what measures they have taken to reduce the risk of bleeding. These might include systems to seal the arterial puncture with a plug of collagen (e.g. Angio-Seal®) and devices which apply direct pressure over the site of the puncture (e.g. FemoStopÔäó)
Bleeding usually presents with bruising or swelling in the groin. However, occasionally if a high puncture has accidentally been made above the inguinal ligament (see diagram), bleeding may not be apparent, because it is retroperitoneal, into the patient’s abdomen or pelvis. The patient may become shocked with a high pulse and low blood pressure and may sometimes have pain or bruising in the flank on the side of the puncture. If bleeding occurs prolonged manual pressure may need to be applied. If the patient is shocked rapid intravenous fluids, blood transfusion or even further intervention may be required.
Less common complications include dissection of the artery or embolism which can cause the foot to become ischaemic. It is therefore very important to check that the foot is a normal colour, temperature and the pulses are present.


