
Every minute counts following a stroke as millions of brain cells (neurones) die as a result of the interrupted supply of oxygen and glucose.
When an artery blocks, initially the nerve cells stop working which causes the symptoms of the stroke. However, unless blood flow is restored the brain cells start to die, causing permanent damage. This process starts within minutes, but can continue for hours.
Patients admitted with stroke within four and a half hours of definite onset of symptoms, who are considered suitable, should be treated with either intravenous alteplase by infusion over one hour usually 0.9mg/kg (up to maximum 90mg) or an intravenous bolus of Tenecteplase 0.25mg/kg. See Additional Information for more details on dosage.
In patients where a CT angiogram shows that a large artery is blocked a thrombectomy may be indicated if it can be done within six hours of a known time of symptoms onset, or where advanced brain imaging suggests it might be effective.
The delay from stroke onset to treatment with thrombolysis and/or thrombectomy should be minimised. Systems should be optimised to allow the earliest possible delivery of treatment within the defined time window.
The chances of a full or nearly full recovery from stroke are much greater the earlier hyperacute treatment is given. This graph shows that the effectiveness of thrombolysis is greatest when given early and reduced with increasing delay between stroke onset and treatment. It may not work at all after 270 minutes (4.5 hours).
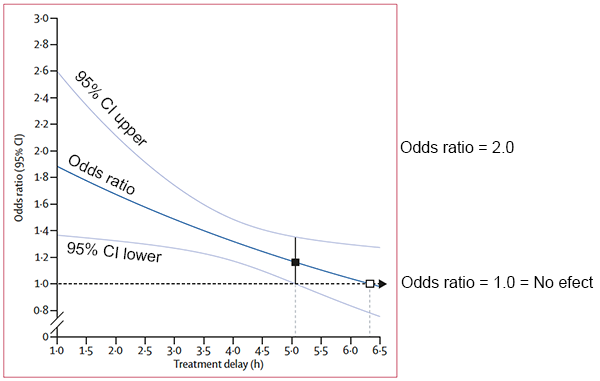
The odds ratio is the odds (or chance) of a good outcome with treatment divided by the odds (or chance) of a good outcome without treatment. An odds ratio of more than one indicates that it will improve patient outcomes. Therefore an odds ratio of two would indicate a doubling of the chance of a good outcome. The 95% confidence intervals (CI) indicate how precise the estimate of effectiveness is. If the confidence intervals do not overlap the one then we are more confident that the treatment is effective.
“The white box shows the point at which the estimated treatment effect crosses 1.0 the line of no effect.
The black box shows the point at which the lower 95% CI for the estimated treatment effect first crosses 1.0 the line of no effect.”
See the full article:
Thrombolysis within 3 hours produced 10 additional good outcomes /100 treated, if the delay was 3-4.5 hours only about 5 good outcomes /100 were achieved – so 5 fewer patients have a good outcome per 100 treated:
A similar relationship between increasing delay and reducing effectiveness is seen for thrombectomy. Thrombectomy within 6 hours produced 40 patients with less disability /100 treated but for every additional hour of delay to thrombectomy – 7 fewer patients have a good outcome per 100 treated.
Advanced brain imaging (see Additional Information) can be used to identify the small proportion of patients who either wake from sleep with symptoms, or who have had symptoms for more than 4.5 or 6 hours, who might still benefit from thrombolysis or thrombectomy respectively.
For more detailed information:
Page last reviewed: 07 Aug 2023


