Contracture
“Is the chronic loss of joint motion due to structural changes in non-bony tissues including muscles, ligaments and tendons”
The Free Dictionary: Medical Dictionary: Contractures
or
“A condition of shortening and hardening of muscles, tendons or other tissue, often leading to deformity and rigidity of joints”
English Oxford Dictionaries: Contracture
Why do contractures develop?
Any joint not moved through its normal range of motion will develop a contracture.
Main factors leading to contractures after stroke are:
- Immobilisation or immobility.
- Spasticity.
- Muscle weakness and paralysis.
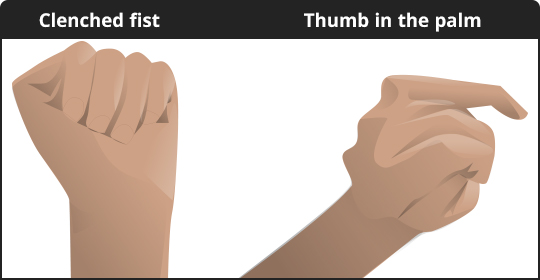
Spasticity does not directly cause muscle contracture, however it does predispose a person resting with muscles in a shortened position.
Relevance for practice
Patients who spend prolonged periods of time with muscles in shortened positions e.g. sitting in a chair all day shortens hip and knee flexors, weakness of the upper limb leads to people sitting with their arms in internal rotation with flexion and pronation.
There also seem to be some people with a predisposition to tendon shortening.
The following good practice principles can help to minimise the negative effects of spasticity:
- MDT assessment and goal planning to include spasticity management.
- Identify and treat any aggravating factors.
- Ensure there is an appropriate 24-hour postural management programme which includes positioning, stretching, splinting if necessary, self-management, carer involvement.
- Ensure there is an appropriate programme of physical therapy and activity.
Page last reviewed: 04 May 2020


