Introduction to anticoagulation
Please note that this Topic Loop is under review and will be updated shortly to reflect the latest National Stroke Guidelines for Stroke (RCP 2023)
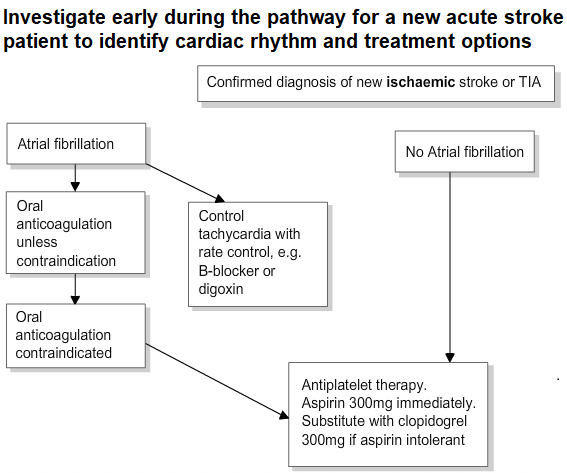
- Anticoagulation may be indicated after an ischaemic stroke if the patient has
- atrial fibrillation
- prosthetic heart valves
- recent myocardial infarction
- deep vein thrombosis or pulmonary embolism
- Anticoagulation reduces the risk of another stroke more than antiplatelets such as aspirin in patients with atrial fibrillation
- Anticoagulation is associated with an increased risk of bleeding
- Warfarin was previously the most commonly used anticoagulant. Warfarin is a vitamin K antagonist and works by inhibiting vitamin K dependent clotting factors. Warfarin requires regular monitoring and it interacts with many other drugs that either increase or decrease its effects. It can be reversed relatively easily if required.
- Patients should be advised to check if any new medications interact with warfarin
- Newer oral anticoagulants have been developed, which may replace warfarin, because they have fewer drug interactions and require less frequent blood tests. They are known as the Direct Oral Anticoagulants (DOACS).
Introduction
There is no ‘safe’ limit of alcohol intake. The risk of developing a range of illnesses increases with any amount you drink on a regular basis.
The Chief Medical Officers’ guidelines for both men and women are: (this applies to adults who drink regularly i.e. most weeks)
- To keep health risks from alcohol to a low level it is safest not to drink more than 14 units a week on a regular basis.
- If you regularly drink as much as 14 units per week, it is best to spread your drinking evenly over 3 or more days.
- If you have 1 or 2 heavy drinking episodes a week, you increase your risks of death from long term illness and from accidents and injuries.
- The risk of developing a range of health problems, including cancers of the mouth, throat and breast, increases the more you drink on a regular basis.
- If you want to cut down the amount you drink, a good way is to have several drink-free days each week.
- If you are pregnant or think you could become pregnant, the safest approach is not to drink alcohol at all, to keep risks to your baby to a minimum.
DOH (2016)