Category: Advancing Modules
Why patients don’t want to take medicines
Adherence
Introduction
There have been a number of terms used to describe how well patients take their medicines. You may be familiar with these:
- ‘Compliance’: can be defined as the ‘extent to which patient’s behaviour matches the prescriber’s recommendation’.
- This term was superseded by ‘Adherence’ which acknowledges that a patient has a choice about whether to accept prescribing advice. It is defined as the ‘extent to which patient’s behaviour matches agreed recommendations from the prescriber’.
- More recently the term ‘Concordance’ has been used. This term too has evolved. Initially it described the position when the respective views of prescribers and patients are incorporated and agreement is reached. However, now it is accepted that concordance requires a wider view. One which stretches from the communication around prescribing decisions to the support that patients require in taking medicines.
It is common for Health Care Professionals to use these terms interchangeably. Despite any confusion this may cause, the objective remains to the same; that patients have optimal benefit from the most appropriate medicine for them.
Topic Loops
Recurring topics in this subject are listed below as topic loops. These are short tutorials explaining key concepts. When working through the cases links to these topic loops will appear at the bottom of the page.
Lower limb orthotics
Ankle Foot Orthosis


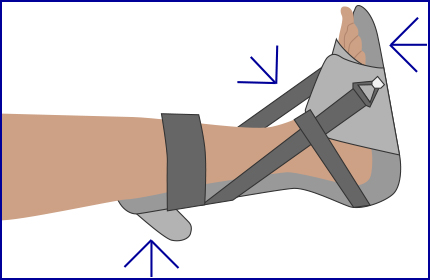
Pressure Relieving Ankle Foot Orthoses (PRAFOs)/Night splints
Knee range of motion orthoses
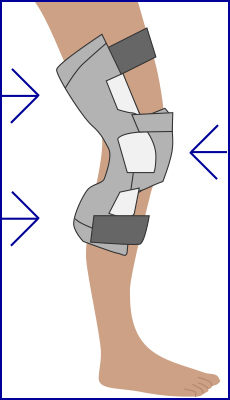
Application of 3 point force
A three-point force system generates a force over a joint to change the angle depending on what is required from the orthosis. This happens when three forces are applied to a body segment, one primary force usually at a joint or where movement is to be either inhibited/facilitated and 2 counter forces above and below this.
Clinical objectives of orthotics
Contracture management
- Maintain/stretch soft tissues
- Relieve pain
- Improve function
- Promote independence
Biomechanical principles
- Identify tissues under increased strain
- Apply forces to reduce pathologic loading to those tissues
- Apply forces to increase chance of creep in shortened connective tissues
- Create rotational equilibrium
- Maximize sagittal and coronal plane biomechanical function
- Realign Ground Reaction Force
- Prevention of excessive range of joint motion
Orthotics
What is an Orthotist?
Orthotists are registered healthcare professionals who specialise in the assessment of the whole body for biomechanical problems and if appropriate may prescribe, measure, fit or review an orthosis.
Orthotics – “The application of external devices (orthoses) to the body. These modify the structural and functional characteristics of the neuromuscular and musculoskeletal systems and are a fundamental part of many rehabilitation programmes.”
WHO definition
The word Orthosis derives from the Greek expression “making straight”.
An orthosis may also be called a “brace”, “splint” or “orthotic”. The purpose and design of an orthosis may change over time along with the changing needs of the patient.
An orthosis can:
- Improve function
- Reduce pain
- Prevent deformity
Maintaining muscle length
Another treatment for tone management which should be done alongside positioning is stretching. This aims to maintain the length of the muscle to prevent shortening and possible development of contractures.
This should only be done after training from an experienced therapist but it can be done by any member of staff and as the patient improves they and their family and carers can be taught safe stretching techniques to maintain position, alignment and muscle tone. Stretching also aids mobilisation of the joints.
Stretching can be applied to a limb by strapping, splints, manual stretching or a combination of all these.
Tips for manual stretching
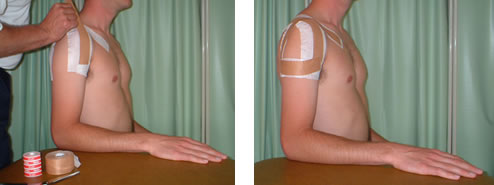
Strapping
Splints or orthoses
Guidelines and recommendations for positioning and spasticity treatment
Physical management to include:
- Active movement, encouraging proximal control, alignment and normal patterns of movement
- Early weight-bearing through both arm and leg
Royal College of Physicians Guidelines
Summary of the recommendations
Click through the slides 1–7 below using the controls ◄ ►
Movement and tone management
If the limb has low tone (Hypotonus), joints should be well supported when moving the limb
If the muscles are high toned (Hypertonus) the joints and limb should be moved slowly.
Irrespective of the tone, when handling the arm adequate alignment of the joints should be maintained throughout the range to prevent damage to rotator cuff muscles i.e. ensure adequate scapular movement and lateral rotation of the shoulder when raising the arm.
Like a stereo the body has to be in balance.
Please enable JavaScript in your browser to see this interactive content.


