Category: Advancing Modules
What is it we are trying to do to manage tone?
Please enable JavaScript in your browser to see this interactive content.
Patient engagement and participation is required at all levels. During the patient’s treatment there may be more than one of the approaches used depending on the patient’s need. For example to facilitate movement in a shoulder, tone management strategies may be done first (stage 1) then the patient and therapist/nurse could work on global positioning (stage 2)
George’s nutrition and hydration status
George currently has an NG tube. This is a form of clinically assisted nutrition/hydration, a term used to describe all invasive methods of delivering nutrients and fluid such as gastrostomy and intravenous fluids. (BPS 2011).
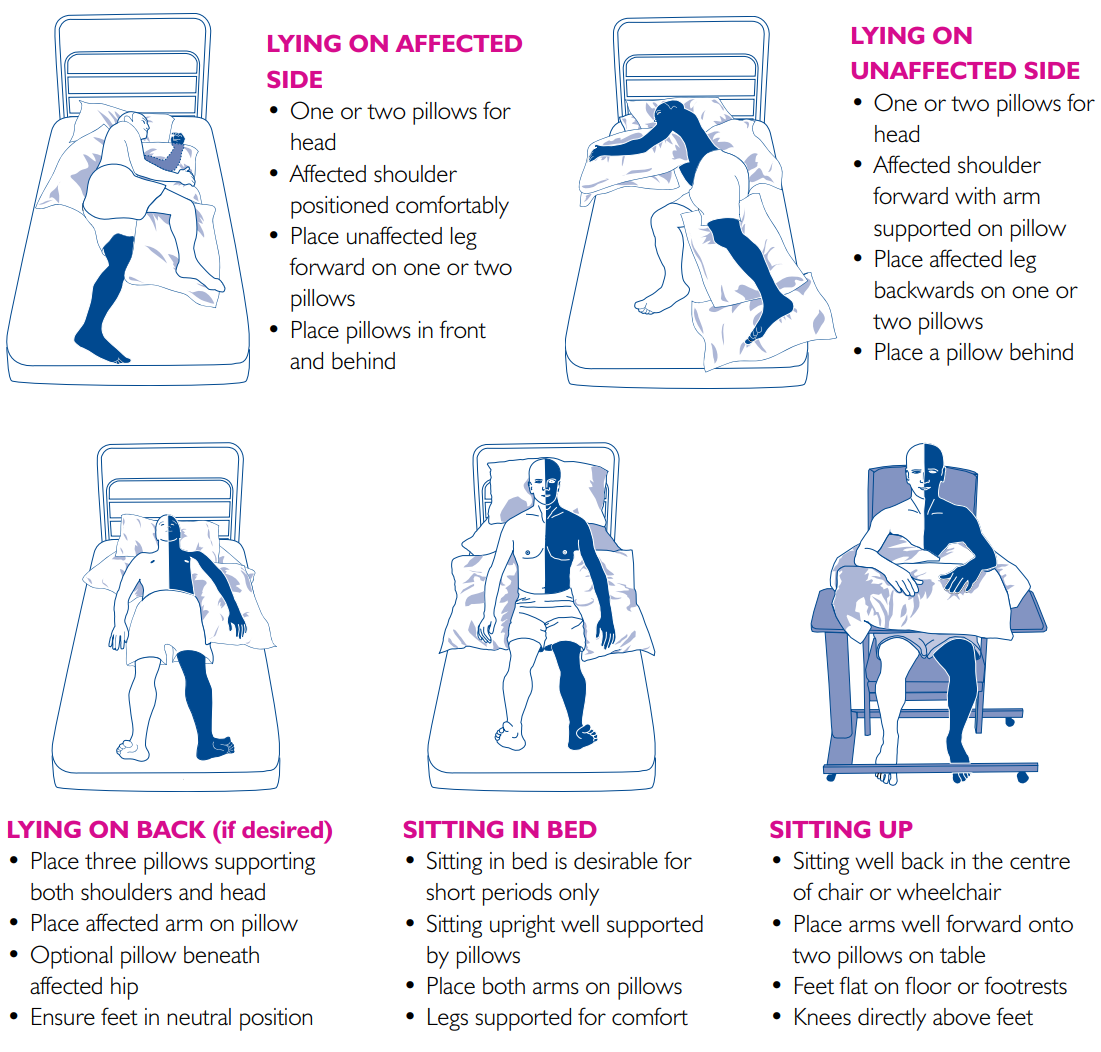
How to position your patient
Select the hotspots on the images below for more information
Positioning for people after stroke
Positioning and base of support
The base of support (BOS) refers to the area beneath an object or person that includes every point of contact that the object or person makes with the supporting surface. These points of contact may be body parts e.g. feet , legs, arms or hands, or they may include things like crutches or the chair a person is sitting in.
Physical support can alter postural tone:
- A larger base of support e.g. lying down, allows greater muscle relaxation and therefore decreases muscle tone
- A smaller base of support e.g. standing up, encourages more activity in muscles and therefore increases muscle tone
By manipulating a patient’s base of support it is possible to alter the patterns of muscle tone.
A larger base of support provides stability where the normal muscle activity is lacking after stroke.
Positions can influence muscle tone:
- Sitting – flexion
- Prone lying (face down) – flexion
- Standing – extension
- Supine lying (face up) – extension
Being in any position for too long will affect tone. Muscles need to be well positioned, regularly stretched and where possible be actively used in normal tasks for tone management to be effective. This will change as the patient starts to recover from their stroke and should be regularly reviewed, plans updated and communicated to staff, patient and carers.
How do we manage tone?
Positioning
The way the patient is positioned and monitored while sitting or lying down can have a significant effect on their tone. Does the person have:
- An appropriate chair or cushion
- An appropriate bed and mattress
- Direct support – using pillows, cushions or tables
- A normal position – some people may need individual equipment such as a splint
- A regular change of position in the care plan
- Regular observation and adjustment as required
- Appropriate pain control if required
For positioning to be most effective there needs to be:
- Staff awareness of tone management plan and good communication
- Patient should be aware if possible of their position and be involved in correcting their position if they are able to comply
- Carer education of positioning, what to do and when to get help
Remember that sudden changes such as coughing, sneezing or laughing may increase tone and change positioning. Look for exacerbating factors.
Exacerbating factors which influence spasticity
Patients with stroke and spasticity often have other exacerbating factors which in turn affect the level of spasticity experienced in their body. Awareness and treatment of these factors is equally important and can make a difference to the overall effect on tone and spasticity. The following are just some of these factors which can be either physical or emotional.
Assessment scales
 There is no universal or ideal assessment measure for hyper or hypo tonus. Your clinical area may use standardised assessments such as Functional Independence Measure (FIM), Barthel Index, Canadian Occupational Performance Measure (COPM) or patient centred assessment. It may be useful to add a simple pain scale for patients with hyper or hypo tonus.
There is no universal or ideal assessment measure for hyper or hypo tonus. Your clinical area may use standardised assessments such as Functional Independence Measure (FIM), Barthel Index, Canadian Occupational Performance Measure (COPM) or patient centred assessment. It may be useful to add a simple pain scale for patients with hyper or hypo tonus.
As a team you should be clear about what you want to measure:
- Self recorded scale e.g. Like the pain scale shown here
- Specific impairment measure e.g. For the shoulder or lower limb
- A specific spasticity measure. In specialist spasticity clinics other assessment scales may be used such as Modified Ashworth Scale, Tardieu or Goal Attainment Scale (GAS) – see specialist clinic section
Importance of treatment
Secondary complications arising from spasticity can:
- Be distressing and painful for the patient
- Be difficult to manage for involved carers & health professionals
- Interfere with rehabilitation and affect outcomes
- Mean that patients with poor functional outcomes usually need more long term care input including for the impact on mental well-being, confidence and depression
- Prevent some patients returning to work activities resulting in loss of income and possible reliance on benefits
- Incur health economic costs increasing the cost of rehab and longer-term care over time. For example the cost of treating a pressure sore due to immobility (per patient) is estimated at between £1,214 up to £14,108 for more severe pressure sores. The complications are also higher in more complex cases. (The cost of pressure ulcers in the UK. Journal of wound care 21(6):261-2, 264,266 June 2012 Dealey C, Posnett J, Walker A.)
Principles of Treatment
- Effective tone management and treatment can prevent long term secondary complications arising
- Spasticity management and treatment is included in multidisciplinary team assessment and goal planning
- Aggravating factors are identified and managed effectively. This can include bladder or bowel discomfort, pain, effects of medication, participation in rehab due to fatigue or other comorbidities pre or post stroke
- An appropriate 24-hour posture management programme including positioning, stretching, splinting as appropriate is agreed and implemented by all staff
- Patient and carer education about the importance of participating in physical therapy and activity programmes and appropriate use of splints if required is implemented. This will help to promote awareness of the importance of tone management and self management strategies
Treat or not?
There are some circumstances where spasticity does not need to be actively treated:
- If spasticity is not having an impact on the patient’s well being or rehabilitation progress
- Spasticity can, in some instances, be used to help function. For example spasticity in the leg may help someone to stand
However, the principles of tone management must still be applied. Remember muscle tone can change over time and therefore requires repeated assessment and management.


