Dr Wood has a medical student with her who has never seen CPSP before. Dr Wood explains to the medical student that CPSP can cause patients a wide range of symptoms and varies according to which part of the brain is affected. She suggests the student look it up on the internet.
See Topic Loop below for further information.
Dr Wood explains to Bob and Jean that there are a number of possible treatments.
Topic Loop:
At the doctors Dr Wood asks Bob about his pain and examines him.
Case notes
Appointment – Dr Wood
|
|
|
Past history: stroke 3 months ago. Osteoarthritis and back pain. Mild chronic kidney disease secondary to long-term use of non-steroidal anti-inflammatory drugs.
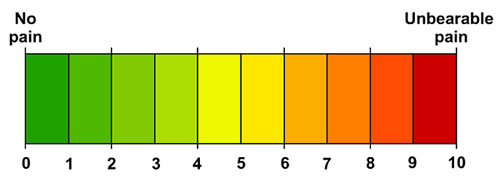
Current problem: burning pain down left side, especially in arm and hand; made worse by anything touching it; keeps patient awake; simple analgesia doesn’t help; feels tired and frustrated – pain affecting quality of life. Scored 10/10 on 10-point pain scale.
Clinical findings: mild left hemiparesis; severe pain on pinprick and cold temperature testing left arm, less severe left leg. No cognitive or language deficits.
Diagnosis: probable central post-stroke pain. |
Dr Wood tells Bob he has central post stroke pain (CPSP). She explains to Bob and Jean what this is and gives them a patient information leaflet: Chest Heart & Stroke Scotland CPSP factsheet [PDF].
Bob tells Bev that he spends a lot of time sitting his armchair in the corner of the room away from any of the things which make his pain worse. He describes this as being in a ‘protective bubble’ and feels isolated and restricted in his activities.
Bev is concerned about Bob and refers him to the doctor for her opinion on what is causing Bob’s symptoms and what the best management plan would be.
Two weeks later the stroke nurse Bev visits Bob at home. His wife Jean has phoned the nurse in advance of the visit to say she is anxious about him. He appears to be in pain and has gradually become withdrawn. Jean feels his mood is low. She has also noticed he has become increasingly sensitive to touch.
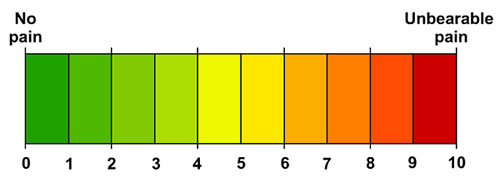
Bev asked Bob to assess his pain on a scale of 1 to 10. The following are two examples of assessment scales:
An example of a Faces Pain Scale: Wong-Baker FACES Pain Rating Scale
An example of a Visual Analogue Scale:
 Bob is 68 years old and is a retired railwayman who loves bowling with his local team. He has had arthritis and back pain for many years, and unfortunately the long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) for pain has led to mild chronic kidney disease. He collapsed at the bowling club and was admitted to the acute stroke unit with left sided weakness.
Bob is 68 years old and is a retired railwayman who loves bowling with his local team. He has had arthritis and back pain for many years, and unfortunately the long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) for pain has led to mild chronic kidney disease. He collapsed at the bowling club and was admitted to the acute stroke unit with left sided weakness.
Bob made good progress with his rehabilitation and his key goal was to return to playing bowls. After 6 weeks in hospital he was discharged home.
Angela is now independent on the ward, her headache is better but she is still quite anxious. The team decide she is ready to be discharged home and Dr Bryce writes a discharge letter to Angela’s doctor.

Dr Mavis Grant
The Health Centre
New Town |
Re: Angela Clark, 2 Rose Garden Drive, New Town
Dear Dr Grant,
Mrs Clark was admitted to the acute stroke unit of New Town Hospital on 1st March with acute onset left sided weakness. CT brain scan showed a haemorrhage in the right basal ganglia. Investigations for an underlying cause identified hypertension but nothing else of note. Glucose and cholesterol were normal. Blood pressure on discharge was 135/75.
She has made a good recovery and is now independent for all ADL activities in the ward. She still requires some further physiotherapy and occupational therapy, which will be provided in her own home.
During her hospital stay, Mrs Clark complained of a persistent headache. This was fully investigated and it appears that the headache was due to the stroke with no other underlying cause. She was prescribed paracetamol with good effect and met with the clinical psychologist who gave her a management plan of how to cope with the pain. The clinical psychologist will continue to see Mrs Clark in her clinic and the Stroke Nurse Specialist will visit her at home and provide her with information about support services.
Mrs Clark was discharged home on 24th April with a care package and rehabilitation at home will be provided by the Community Stroke Team. I will see her at the stroke clinic in 6 months time to review her long term medication requirements and in the meantime would be very grateful if you could monitor her blood pressure.
Medication on discharge:
Paracetamol 1g qds
Amlodipine 10mgs od
Ramipril 5mg od
Yours sincerely
Dr Kenneth Bryce
Stroke Consultant |
The clinical psychologist meets Angela and asks her about her headache and how it is affecting her. She gives Angela information on post-stroke headache and discusses strategies to help Angela manage her pain and anxiety. The psychologist then gives the MDT a plan on managing Angela’s symptoms.
MDT Action Plan
|
 |
|
Distraction
- try to engage her in the kinds of activities she usually enjoys
- get her to take part in tasks in therapy
Clear rehab goals
- focus on goals of getting home and back to doing the things she enjoys
Relaxation
- encourage her to take part in relaxation therapy – likely to help since if she is tense and anxious that may exacerbate her headache
Education
- ensure she understands that there is nothing sinister underlying her headache
- reassure her that although rehab activities may increase her headache at the time this does not mean they are harmful
Involve her family in rehab
- provide her family with information about headache after stroke
- encourage them to work with her in rehab and in managing her pain
|
Click on the plus symbols in the graphic to find out more:
See topic loop below for further information on mood screening.
Topic Loop:
Nurse Moffat tells Dr Bryce that she thinks Angela should have analgesia prescribed for her headache. Dr Bryce considers what he might prescribe.