- Can be worn on the bare leg or over pyjamas or thin trousers
- Lay flat under leg, then wrap around
- Tight enough, so just two fingers can fit underneath sleeve at knee

The following video shows the correct application of the IPC sleeves.

The following video shows the correct application of the IPC sleeves.
The CLOTS 3 trial only tested SCD Express thigh length sleeves. We have no information in stroke patients about the effectiveness of compression of the calf or foot only.
| Sizing the SCD express sleeves | |
|---|---|
| Thigh circumference | Size of sleeve |
| < 16 inches, 40.6 cm | X small |
| 16-22 inches, 46-56 cm | Small |
| 22-28 inches, 56-71 cm | Medium |
| 28-36 inches, 71-92 cm | Large |
The following video illustrates how to size Kendall’s SCD IPC sleeves.
The CLOTS 3 trial only tested IPC for the first 30 days because this is the period when the risk of DVT is highest. It is generally recommended to remove IPC at 30 days. However, if the patient remains immobile beyond 30 days and then becomes unwell with infection or dehydration it would be logical to re-apply IPC until these additional risk factors have been effectively treated. This strategy has not been tested in a randomised trial.
IPC is suitable for:
IPC is not suitable for:
A number of manufacturers produce IPC devices. The devices are of different types and vary in ways which may influence how effective they are.

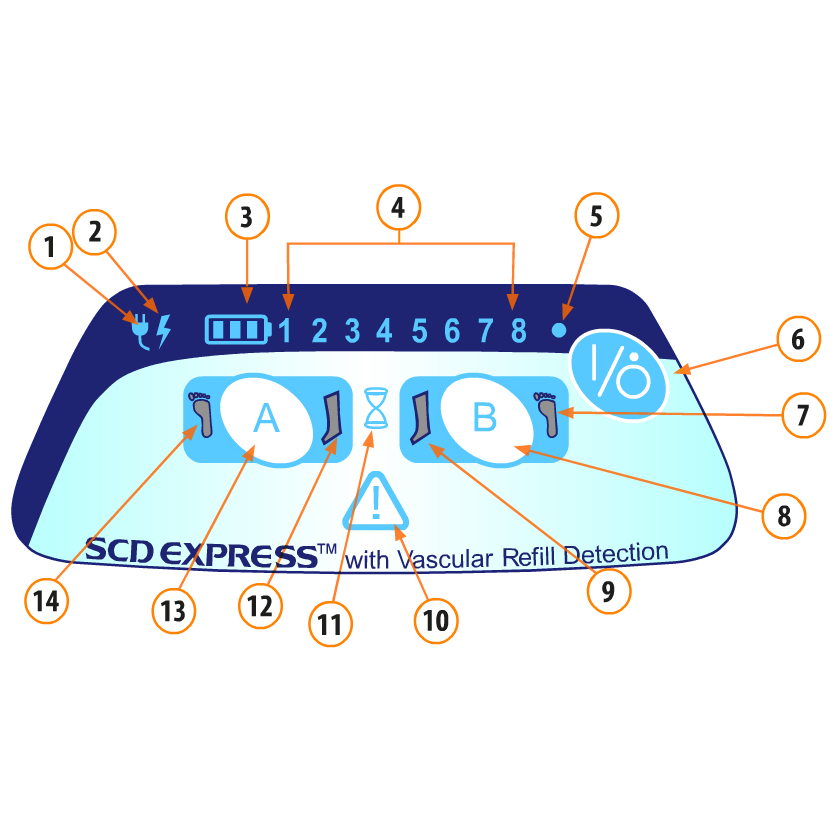
The CLOTS 3 trial tested the Kendall SCD Express system
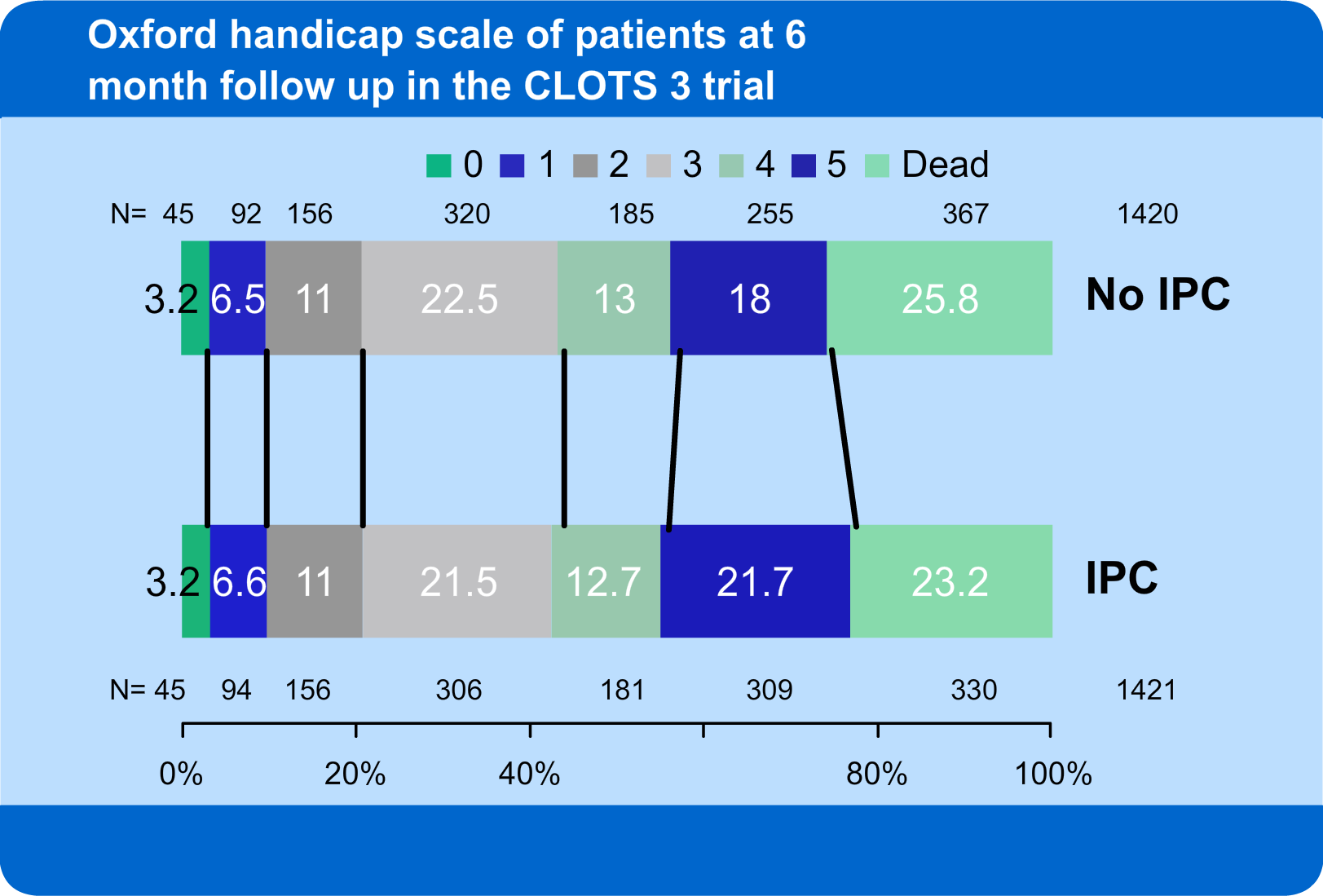
The Oxford handicap scale is a measure of disability, ranging from 0 (no symptoms) through to 5 (bed-bound and incontinent) and 6 (dead). There was no statistically significant difference in the Oxford handicap scale between those allocated IPC and No IPC. However there is a 3% reduction in the proportion who have died at the final follow up in the IPC arm. Also there is a 4% increase in the proportion surviving with severe disability with IPC. This issue is discussed in the Lancet neurology paper.
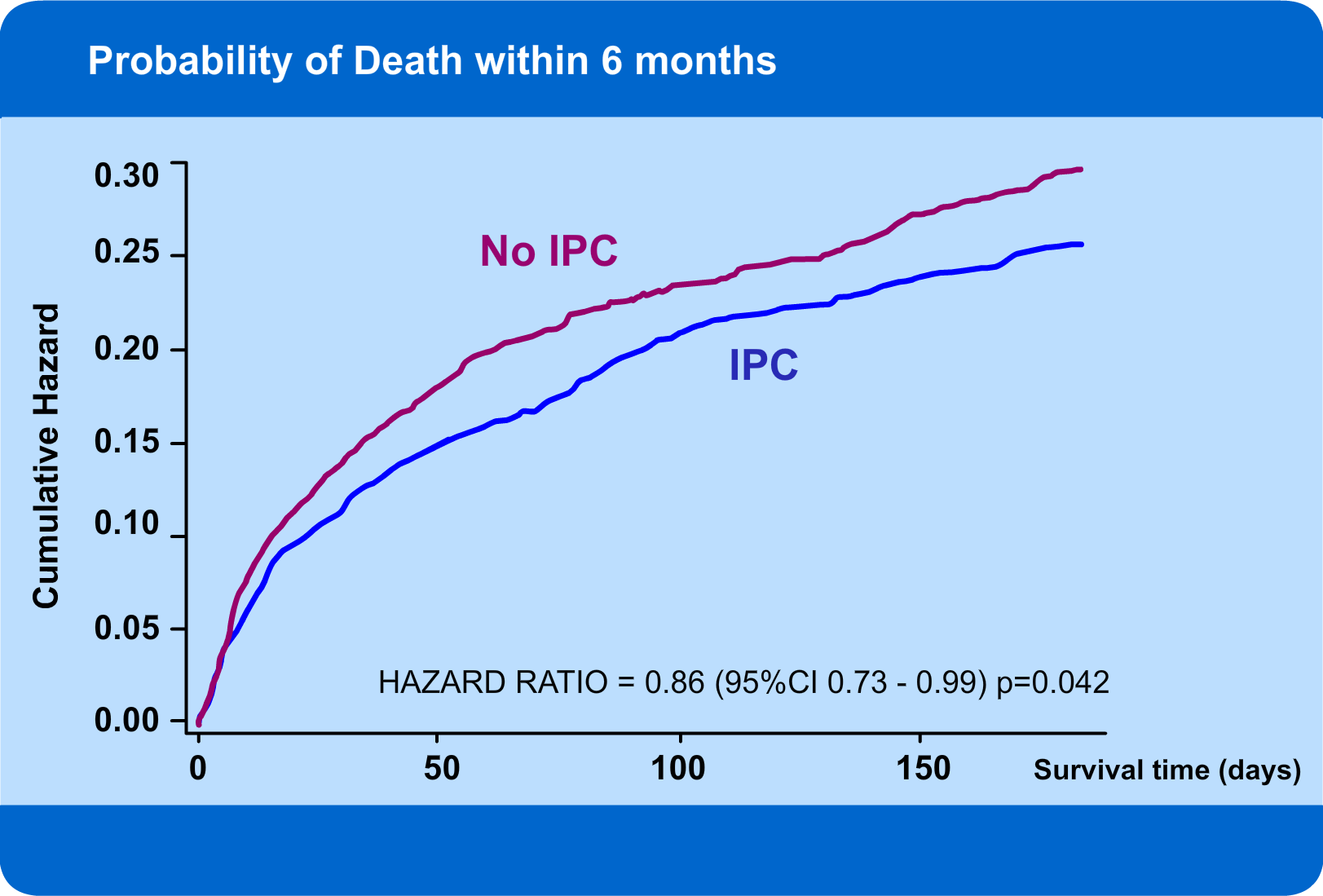
Patients allocated IPC had a lower hazard of death (increased chance of survival) during the first six months after enrolment compared to those allocated to routine care.
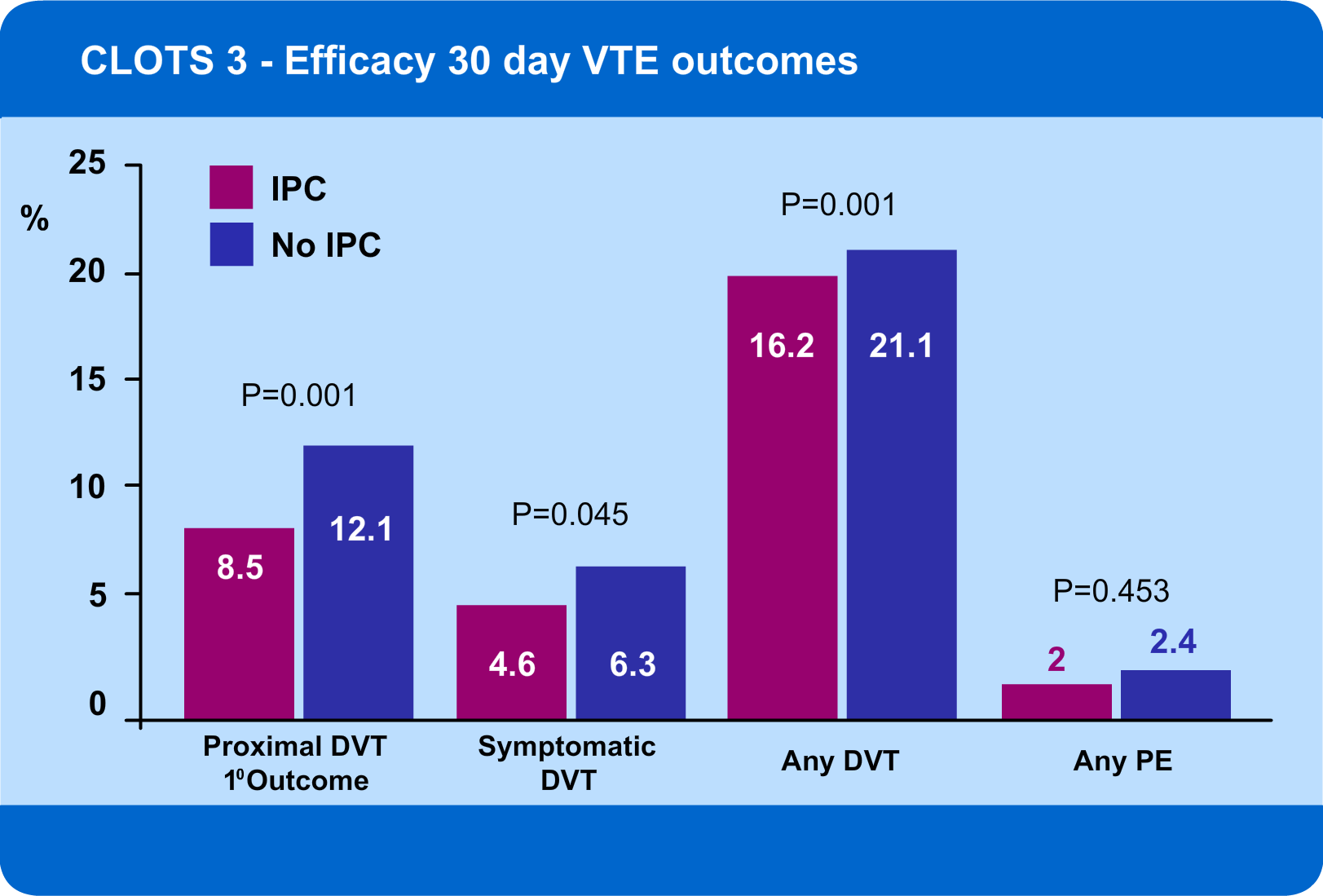
Patients allocated IPC had a reduced risk of: