Iain’s pathway
Methods to prevent bleeding:
If artery is punctured above inguinal ligament severe bruising may not be visible in the groin – it may track upwards, causing retroperitoneal bleeding and present with hypotension and shock.
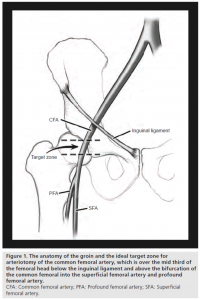
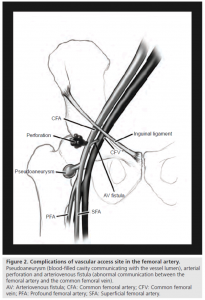
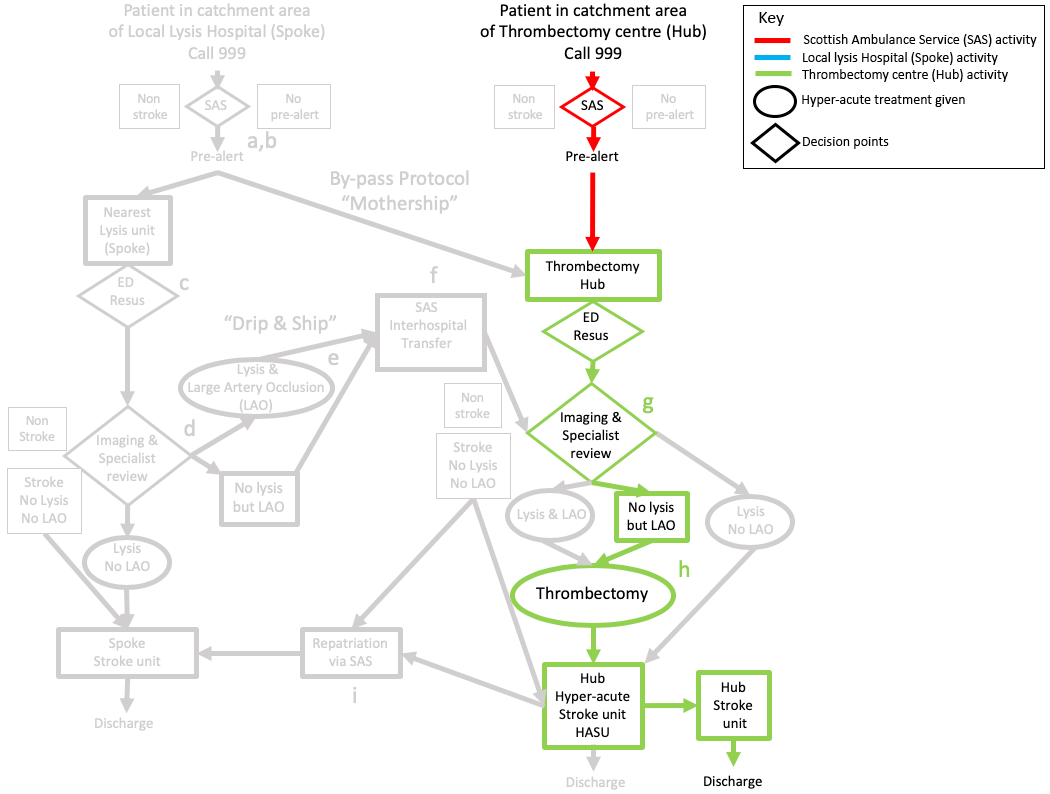
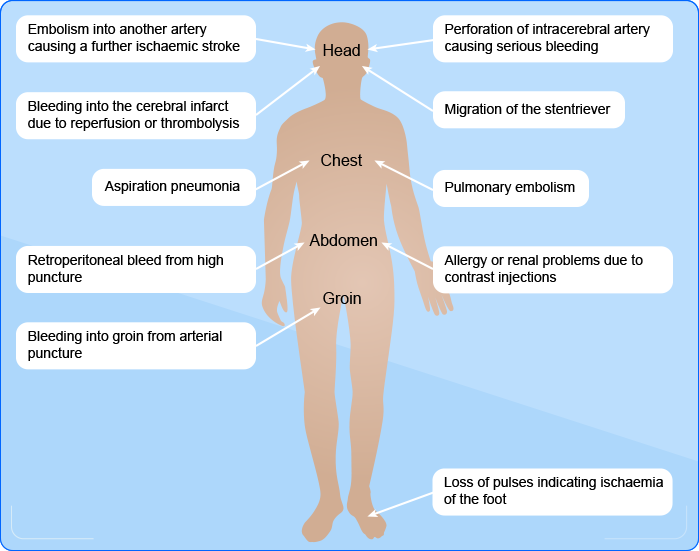
“Figure 1. The anatomy of the groin; Figure 2. Complications of the fermoral artery” Shaun Bhatty, Richard Cooke, Ranjith Shetty, Ion S Jovin and Mary Beatty-Brooks is licensed under CC BY 4.0
Iain is monitored with frequent NEWS and NIHSS, in a similar way to patients who have had thrombolysis. However, the team need to be alert to some additional serious complications – in particular at the arterial puncture site, which is usually in the groin. This is even more likely in patients who have had thrombolysis or, like Iain, are taking oral anticoagulants.
The team phone his wife to explain that he has had a serious stroke due to a blocked artery.
Although Iain cannot have thrombolysis because he has taken Apixaban he is eligible for thrombectomy which needs to be done as soon as possible – his wife tells them to proceed and she will come to the hospital.
The interventional radiologist is alerted and prepares their team. Iain has a general anaesthetic (2-3 hours post last meal) because Iain does not understand what is happening and is agitated and unlikely to stay still.
The stroke nurse stays with Iain and greets his wife when she arrives at the hospital, explaining what is happening. She gives her a leaflet about hyperacute treatment.
Information for patients re acute treatment including thrombectomy [.pdf, 319KB]
Iain undergoes a thrombectomy. For more details on thrombectomy see: Introduction: What is a thrombectomy?
The team successfully re opens his left middle cerebral artery using both a stentriever and suction catheter. Iain is moved to recovery area at 11.45am and is then moved to the hyperacute stroke unit (HASU) at 12.30 when he is fully alert. There he can be closely monitored to detect possible complications.

At 10.45 they arrive at the ED and take him straight into resus where the medical team are waiting for him.
The medical team confirm the time of onset with the paramedics and phone Steve to check that Iain was perfectly well prior to the 3rd hole.
They phone Iain’s wife who confirms that he is on Apixaban, and took his tablets at 8am after breakfast.
They carry out a rapid neurological assessment based on the NIHSS to confirm the diagnosis of a left hemisphere stroke.
Enter Iain’s NIHSS score based on the finding on his neurological examination described below.
Iain is alert, but does not follow any commands and cannot say the month or his age. He has a right visual field defect in both eyes, no movement in right arm or leg and does not respond to painful stimulus on the right arm and leg.
See the NIH Stroke Scale:

At 10am he is on the 3rd tee when his playing partner, Steve sees him develop a right facial droop, fall to the ground and is unable to rise. His speech is incomprehensible.
Steve recognises the signs of a stroke and dials 999 on his mobile.
At 10.20 the ambulance arrives, via the cart track, the paramedics carry out the FAST test (face drooped, unable to lift right arm, unable to speak), check his BM which is normal, and his blood pressure is 178/95. A rhythm strip confirms atrial fibrillation.
For more on the FAST test:
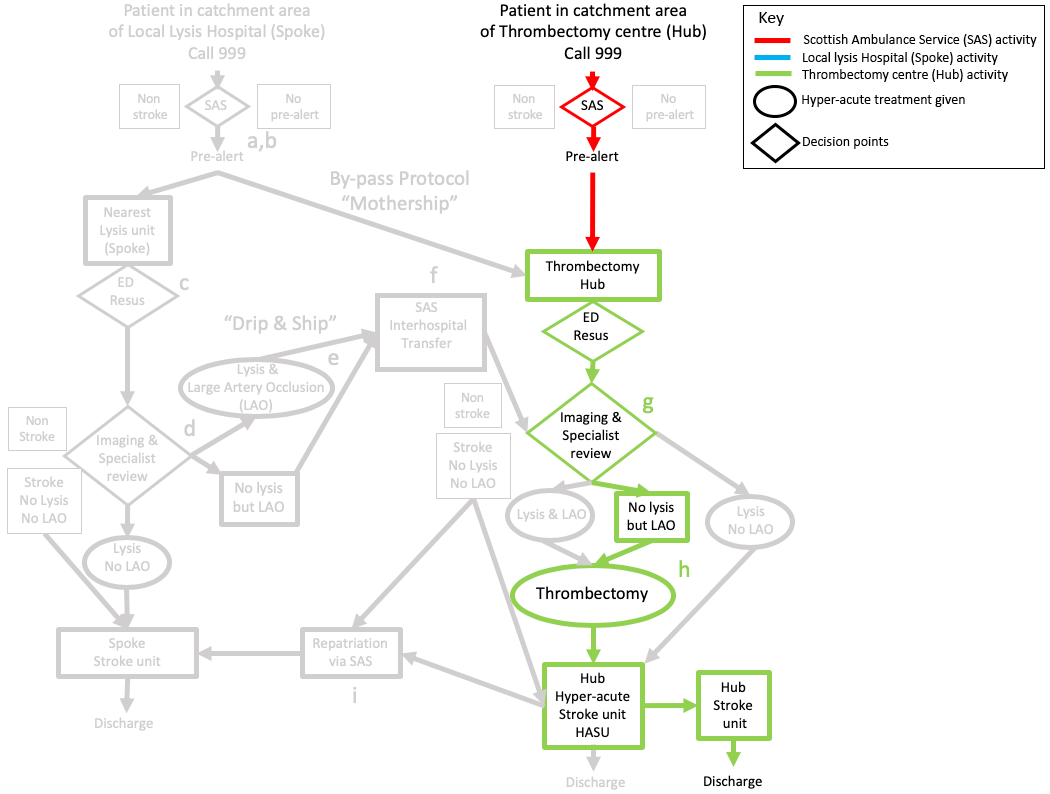
At 10.30 they leave the scene and pre-alert the emergency department (ED) at their local hospital which is a thrombectomy hub i.e. able to offer both thrombolysis and thrombectomy.


Iain is an 81 year old, retired joiner who lives independently with his wife, playing golf twice a week. He is in good health although has raised blood pressure and atrial fibrillation. He is on Bendroflumethiazide and Apixaban.
