Both patients have been discharged from hospital.
Vince has gone back to betting on his horses and, although he still struggles slightly with reading, is showing good recovery. He has a good understanding of his defect and uses compensatory strategies well.
Nigel has given up on reading as well as playing golf and is still largely unaware of his symptoms. His family and friends are aware of his defect and make the appropriate adjustments.
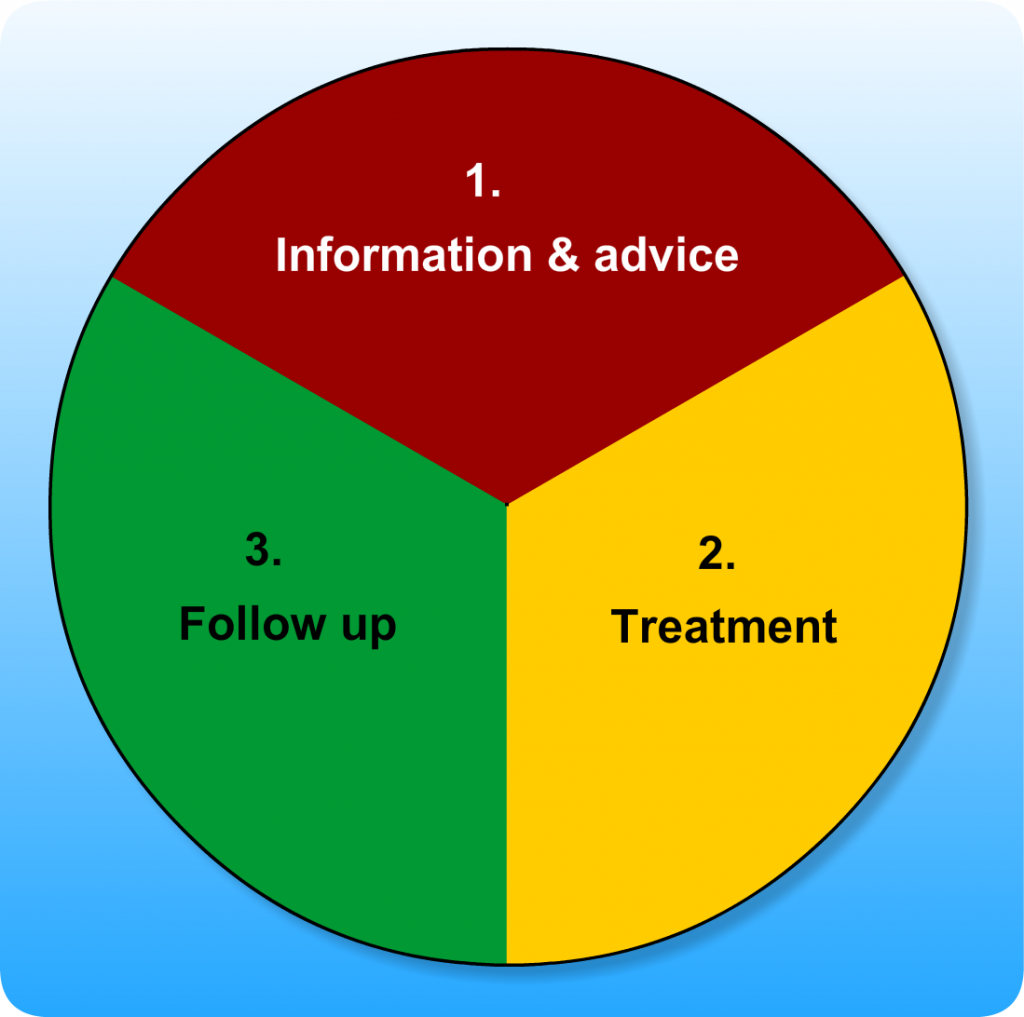
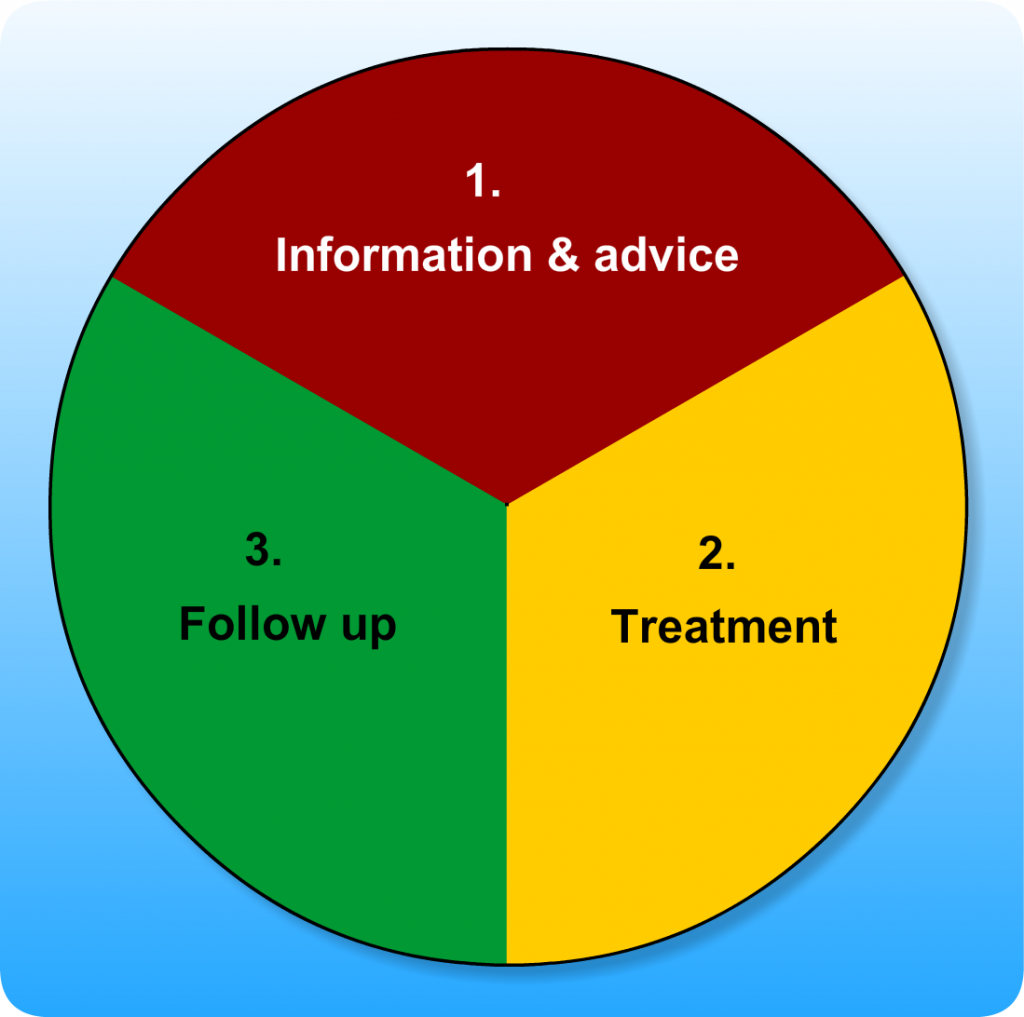
If patients have persistent visual problems following stroke, clinicians should be aware of the additional sources of assessment, treatment and support.
Sight impairment registration
Sight impairment registration due to visual field loss is determined by the extent of visual field loss combined with the level of central vision. An ophthalmologist is the only person that can register someone partially sighted, therefore referral to the eye department should be organised if the patient may be eligible and they are keen to be registered. The benefits of registration can be highlighted to patients by the Royal National Institute of Blind People (RNIB) website, but one of the most important aspects is help with travel if a person can no longer drive.
Registering your sight loss
Driving guidelines
Patients should be provided with information regarding driving suitability. Patients with visual neglect and those with significant visual field loss are not permitted to drive.
If there is any query regarding driving suitability, patients should be advised to contact the DVLA. The DVLA will initiate a specific visual field assessment (called an Esterman visual field test) at a local optometrists and inform the patient if they are still permitted to drive.
Access to social services
If patients are registered as partially sighted, social work departments are notified of this and a home environment assessment is undertaken. This may be a carried out by sensory impairment teams. However, if patients are not keen to be registered, any individual can request a home environment assessment directly from the social work department.
Other sources of help in the community are:
There are other agencies that can offer support after the patient is discharged from hospital. These include:
- Local and national visual impairment organisations
- Local and national stroke support organisations
- Local authority/social work sensory impairment services
- Vocational rehabilitation services
Contacts:
Local societies for the blind in Scotland who work specifically with people affected by sight loss after stroke:
There will be equivalent services in your local area.
Generally people with visual field loss have a greater awareness and understanding of their defect than those with visual neglect. As a result, treatment options for visual field loss tend to be more effective than those available for visual neglect. Insight is key to a patient compensating for the field loss or neglect, so treatment should be combined with education to increase awareness for both the person and their carers/family and encourage self-management.
Reading is commonly affected in both visual field loss and neglect as the ability to smoothly follow a line of text is disrupted. Targeted treatment strategies are important to include.
Trials and ongoing research
Research into the most effective treatments for visual field loss and visual neglect is ongoing. At present, there is limited high quality evidence on which to base practice, but some useful sources of information are:
Cochrane Reviews:
- *Neglect: Cognitive rehabilitation for spatial neglect following stroke | Cochrane
- Field loss: Interventions for visual field defects in people with stroke | Cochrane
- Eye movement: Interventions for eye movement disorders in people with stroke | Cochrane
*an update of this review should be published in 2021.
National Clinical Guidelines for Stroke:
Royal College of Physicians (2016): Stroke guidelines
Vince has left visual field loss (also called left homonymous hemianopia). Nigel has left visual neglect and also a possible left visual field defect.
| What information and advice would you give? |
| 1. Visual Field Loss |
- The patient should be advised that they have visual field loss – they may not be aware of their visual problems nor that it affects both eyes. This information can help them develop their own coping strategies.
- The diagnosis and explanation should be provided by appropriately trained staff. They may explain what visual field loss is, how it has occurred, and its possible effects on function and the likelihood of recovery.
- The effects on patients’ functional abilities on the ward can include:
- Difficulty with mobility due to bumping into obstacles or people
- People may be more likely to fall
- Problems reading
- Difficulty with activities of daily living e.g. personal care and feeding
- Carers and family should be advised to approach patients initially from their non-affected side and to position objects of interest e.g. food and TV, to their non-affected side. Once they are aware of the person/object the patient can be encouraged to scan to their affected side.
|
| 2. Visual Neglect |
- An accurate diagnosis and explanation should be given by appropriately trained staff. Staff should explain what neglect is (and also possible coinciding field loss) and its effects on function.
- Neglect patients commonly have a poor understanding of their visual problems and it is therefore important to explain the defect to family and carers too.
- Family and carers should approach the person in the area they are attending to and encourage attention to the neglected side by moving gradually to the affected side and by speaking and presenting objects on this side. The purpose is to try and improve the patient’s awareness of the neglected side (often to their left).
- If giving stimuli predominantly to the neglected side causes anxiety, stimulation should be given more equally to both sides.
|
| 3. Visual Field Loss and Visual Neglect |
- Staff should be advised of the visual problems and they should be noted clearly in the patients case records.
- Advice should be provided to all drivers. Patients who suffer from a stroke, irrespective of impairment, are not allowed to drive for a period of 1 month. (See below for further information)
|
This information and advice can be reinforced and supported by other resources:
General Information:
Chest, Heart & Stroke Scotland: Visual problems after a stroke [PDF]
Visual Field Loss:
British and Irish Orthoptic Society: Stroke Visual Field Loss leaflet. (PDF, 72 KB)
Visual Neglect:
British and Irish Orthoptic Society: Stroke Visual Inattention leaflet (PDF, 27KB)
Driving:
Chest, Heart & Stroke Scotland: Essential Guide to Driving with a medical condition [PDF]
The Stroke Association: Driving after stroke [PDF]
What should we do now that we have identified their visual problems?
Functional assessments are used to assess motor, sensory, cognitive, psychological and social skills and the effect of any impairment on the performance of tasks.
It is common for occupational therapists to assess a person’s ability to carry out daily living activities, such as self care and domestic tasks as well as work and leisure activities.
As we think Vince and Nigel may have visual problems, the team decides they should look at how this affects function, by assessing how they perform a dressing task. The following link describes how to set up a dressing task: How to set up a dressing task [PDF, 24.6 KB]

How did Vince and Nigel get on?
Vince
- With time and some initial prompts, Vince turned his head, reached out to the left with his left arm and found all clothing items as they were required.
- Once he found each clothing item, Vince would hold it up to his right side to position it correctly to put on.
- Vince struggled to use the mirror, but by turning his head was able pull his jumper completely over his left shoulder.
Nigel
- Nigel did not find any of the clothing items on his left and when cued to find the missing items and turn his head, he responded but only for a short time, refocusing on items within the range of his right side.
- Nigel struggled to position the garment properly and started dressing with the sleeves tangled up.
- The mirror appeared to have no impact on Nigel’s ability to adjust his jumper and it continued to be snagged on his left shoulder without him noticing.
For further information on functional assessment see the Additional Information box.
The patient should then undergo tests for eye movement problems, visual field loss and visual neglect. Assessment of eye movements is covered in detail in one of the other scenarios in this module.
Visual field loss
Read the PDF file and then watch the video clips.
How to carry out a Confrontation Visual Field Assessment [PDF, 86KB]
Visual neglect
Read the PDF file and then watch the video clips.
How to carry out a Visual Neglect Test (Line Cancellation Test) [PDF, 38KB]