Following review of the evidence the team developed a Local Action Plan to improve their performance in meeting this standard. (See the Improving patient care topic loop below for further information.)
Action Plan
Reporting document for patients with stroke having swallow screen within 4 hours of admission to hospital. (National Standard = 100%)
| 2021 data |
Feb 2022 |
March 2022 |
Barriers |
Agreed Actions |
Timescale/Lead person |
| 60% |
42% |
40% |
Poor recognition/diagnosis of stroke in the emergency department, and general lack of awareness of the need to swallow screen all confirmed or suspected stroke patients regardless of severity. |
Twice daily visits to A&E/ medical receiving to ensure swallow screening is performed and documented in the afternoon and late evening. |
Stroke Senior Charge Nurses – ongoing |
| Poor documentation of swallow screen assessment; including lack of understanding of how to record swallow screen status of an unconscious patient.
|
Monitoring of training and education of all staff involved in swallow screening e.g. core competency course and onsite training sessions by Speech & Language Therapy to emergency care and stroke unit staff. |
Stroke Senior Charge Nurses – ongoing
Stroke Senior Charge Nurse – ongoing
SLT – ongoing |
| Poor documentation of swallow screen assessment; including lack of understanding of how to record swallow screen status of a unconscious patient.
|
Ensure all day and night nursing staff are swallow screen trained. |
Senior Charge Nurse – ongoing |
| Reinforcing the need for the nurse to clearly document whether a patient is safe or unsafe to swallow; and where the patient is unconscious document that this status makes them unsafe to swallow.
Use of sticker to highlight outcome of swallow screen. |
Senior Charge Nurse – ongoing |
Topic Loop:
Dr Morrison and Charge Nurse Bond work in the stroke unit of the hospital and receive monthly reports from the Scottish Stroke Care Audit to update them on performance against nationally agreed standards for stroke care. (See the Clinical standards and Clinical audit topic loops at the bottom of the page for further information.)
When they received the monthly report in March they were disappointed as they felt that the data presented did not reflect their performance in relation to swallow screening of the patients in their ward.
They raised this matter at the outset of their review with the Action Plan and SSCA Coordinators. They said that all stroke patients have a swallow screen when they are admitted to the stroke unit as per the guidelines and that the nurses know it should be clearly documented in the patients’ records.
The Action Plan and SSCA Coordinators explained that the national standards and criteria for swallow screening stipulates that swallow screening should be performed on day of admission not the day the patient was admitted to the stroke unit. Therefore if patients don’t come to the stroke unit until the day following admission they should have their swallow screen done in the medical receiving unit (or other medical ward) and this should be clearly documented.
Charge Nurse Bond said she had not been aware that this was the case and decided to look at the national standards & criteria and the research / evidence behind this. She refers to the following:
Topic Loops:
The national standards and criteria stipulate that all patients should be screened by a standardised assessment method to identify any difficulty in swallowing safely. The new swallow screen standard (2016) means this should be carried out within 4 hours of admission to hospital and before the patient is given any food/drink/oral medication. It should be clearly documented that this screen has been carried out and what the results of the screen are.
The graph below shows the results produced in March 2022 from the Scottish Stroke Care Audit. NHS Boards receive monthly reports to monitor performance against standards and where needed instigate changes that ensure the highest quality care is given to patients.
The graph below shows the results produced from the Scottish Stroke Care Audit.
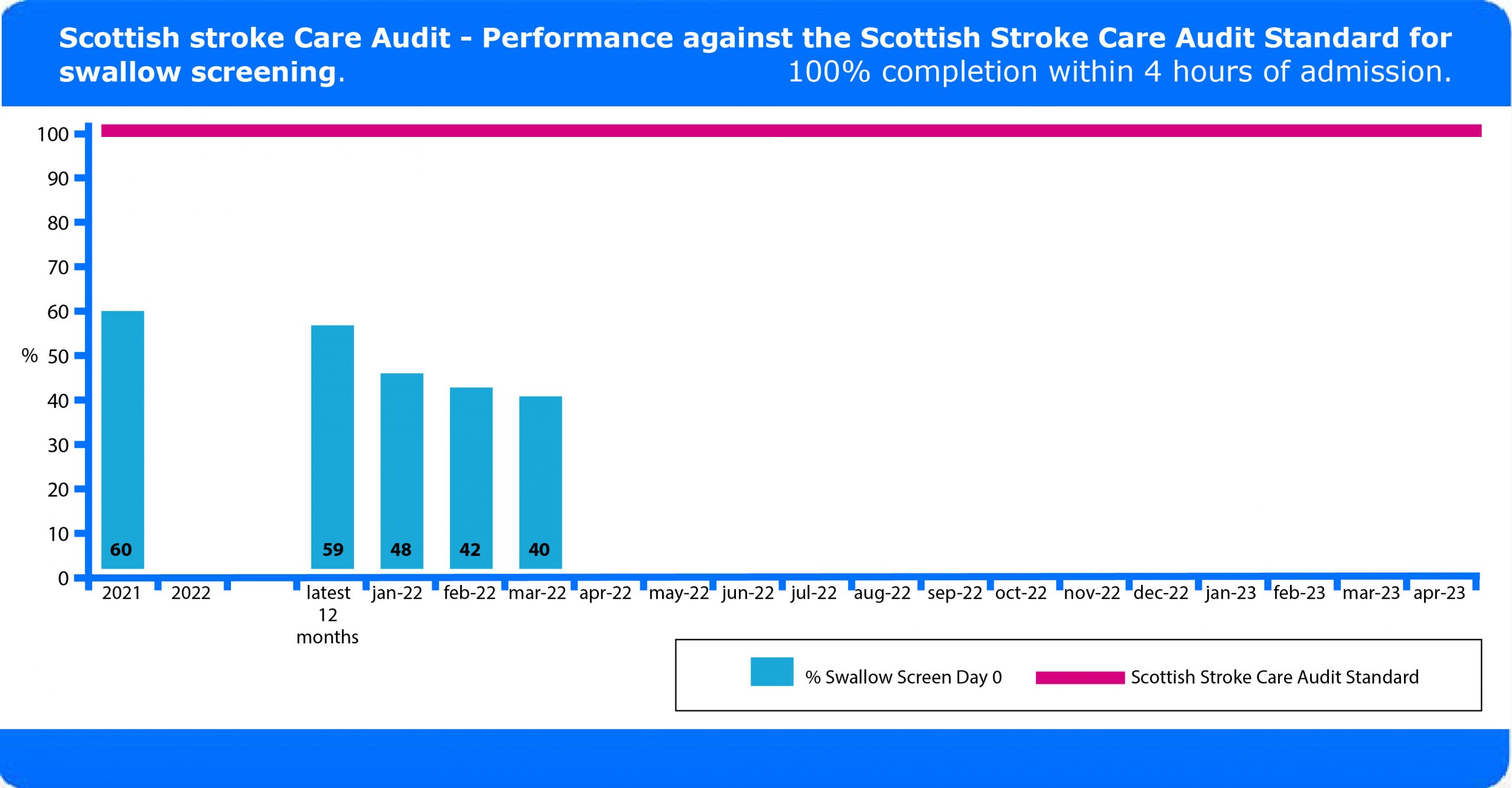 You can see from this graph that the target of 100% of patients having a swallow screen is not currently being achieved in this Health Board. (See ‘Clinical audit’ topic loop at the bottom of this page for further information.)
You can see from this graph that the target of 100% of patients having a swallow screen is not currently being achieved in this Health Board. (See ‘Clinical audit’ topic loop at the bottom of this page for further information.)
Topic Loop:

 Thomas is a 43 year old builder who self presented at the A&E department of his local hospital. He arrived at 7.30am having woken that morning with right arm weakness and slurred speech. He was assessed in the A&E department and then admitted to the medical receiving unit for further investigation. The diagnosis of stroke was confirmed by a CT scan which showed an infarct, he remained in the medical receiving unit and was transferred to the stroke unit the following day.
Thomas is a 43 year old builder who self presented at the A&E department of his local hospital. He arrived at 7.30am having woken that morning with right arm weakness and slurred speech. He was assessed in the A&E department and then admitted to the medical receiving unit for further investigation. The diagnosis of stroke was confirmed by a CT scan which showed an infarct, he remained in the medical receiving unit and was transferred to the stroke unit the following day.
A nurse in the stroke unit noted that Thomas was coughing and she checked his medical records to see if a swallow screen had been carried out. There was no evidence of this in Thomas’ records although it did state that he had eaten his breakfast. The nurse carried out a swallow screen, which Thomas failed. Thomas was referred to speech and language therapy for further assessment and he was informed that he should not eat or drink until this had been carried out. (See the Clinical standards topic loop below for further information.)
Topic Loop:
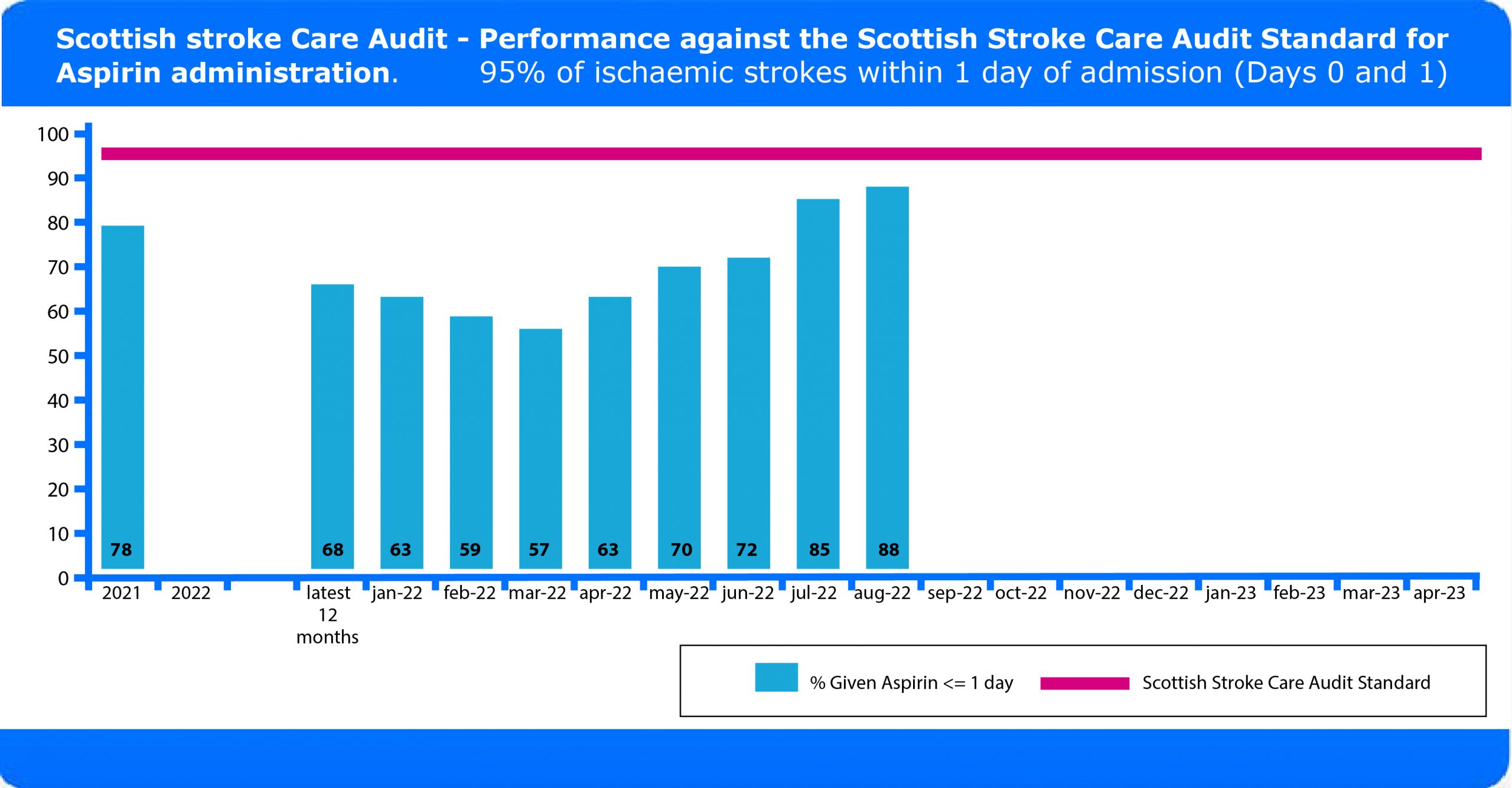
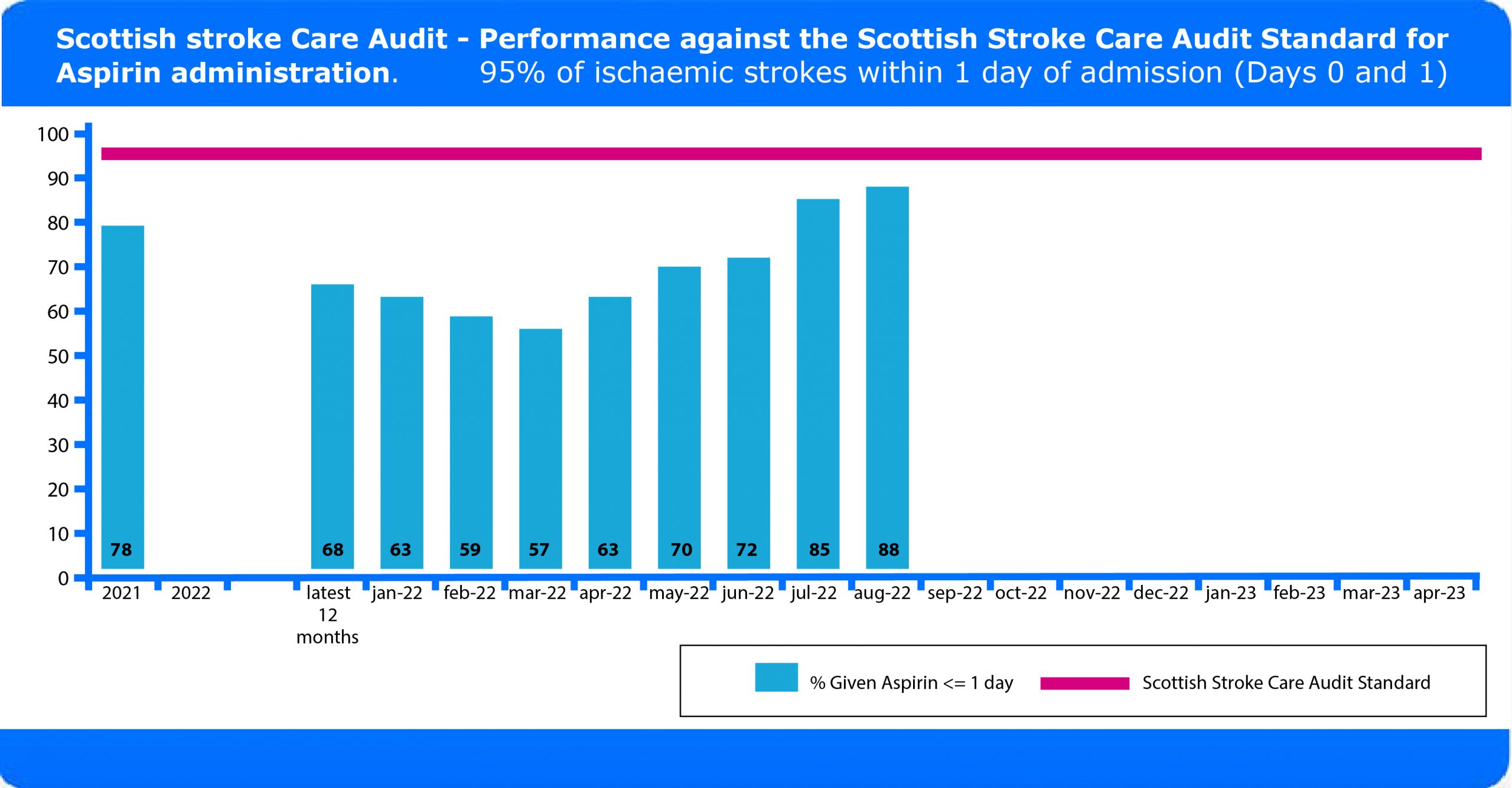
Over the next several months Dr Porter and colleagues continued to implement their local action plan and received monthly reports from the SSCA. The graph below shows the improvements they made in prescribing aspirin for acute ischaemic stroke patients over that period.
Doctor Porter and his colleagues used the evidence to devise a local action plan to improve their performance in meeting this standard. Below is the action plan they developed. (See the Improving patient care topic loop below for further information.)
Action Plan
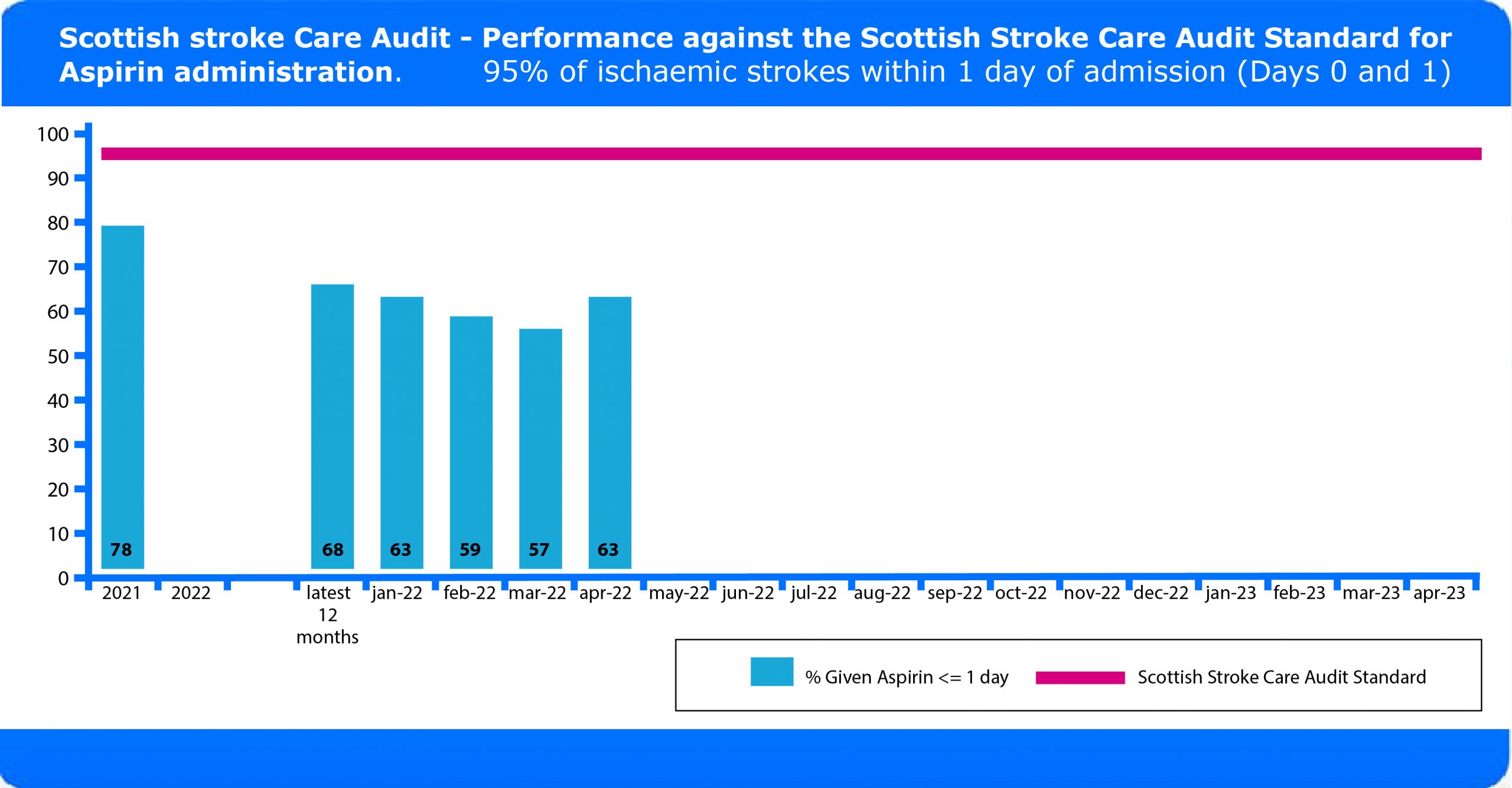
Reporting documents for patients with ischaemic stroke receiving aspirin on the day of admission or day after. (National Standard = 95%)
| 2021 data |
Feb 2022 |
March 2022 |
Barriers |
Agreed Actions |
Timescale/Lead person |
| 78% |
59% |
57% |
Poor recognition/ diagnosis of stroke in the emergency department, and general lack of awareness of the need to administer aspirin to ischaemic stroke patients. |
Twice daily visits to A&E/ medical receiving unit to advise on prescribing and administration of aspirin after an acute stroke. |
Stroke Senior Charge Nurses – ongoing |
| Lack of understanding by junior medical staff of the need to promptly access CT scan results; to allow prescription and administration of aspirin. |
Stroke unit nurses to check aspirin has been prescribed and administered. |
Stroke Senior Charge Nurses – ongoing |
| Lack of understanding of the need to use aspirin and not alternative antiplatelets in the acute management of ischaemic stroke. |
Stroke unit nurses to check aspirin has been prescribed and administered.
Junior doctor training. |
Stroke Senior Charge Nurse – ongoing
Lead stroke clinician – ongoing |
Topic Loop:
Dr Porter and nurse Cameron raised the matter of administration of aspirin at the outset of their review meeting with the Action Plan and SSCA Coordinators. Dr Porter said that both aspirin or alternative antiplatelets were being prescribed to all ischaemic stroke patients as per the guidelines. The Action Plan and SSCA Coordinators explained that the Stroke standards measure only against the use of aspirin, and no other antiplatelets.
Dr Porter had not been aware that this was the case and decided to look at the Stroke standards and the research/evidence behind this. He refers to the following:
(See all the topic loops below for further information on the above.)
Having done this Dr Porter and Charge Nurse Cameron agreed to set up a local action plan to make improvements in the administration of aspirin on their ward.
Topic Loops:
The national standards and criteria stipulate that aspirin treatment should be initiated on the day of admission or the following day and continued for all patients in whom a haemorrhagic stroke, or other contraindication, as specified in the national audit, has been excluded.
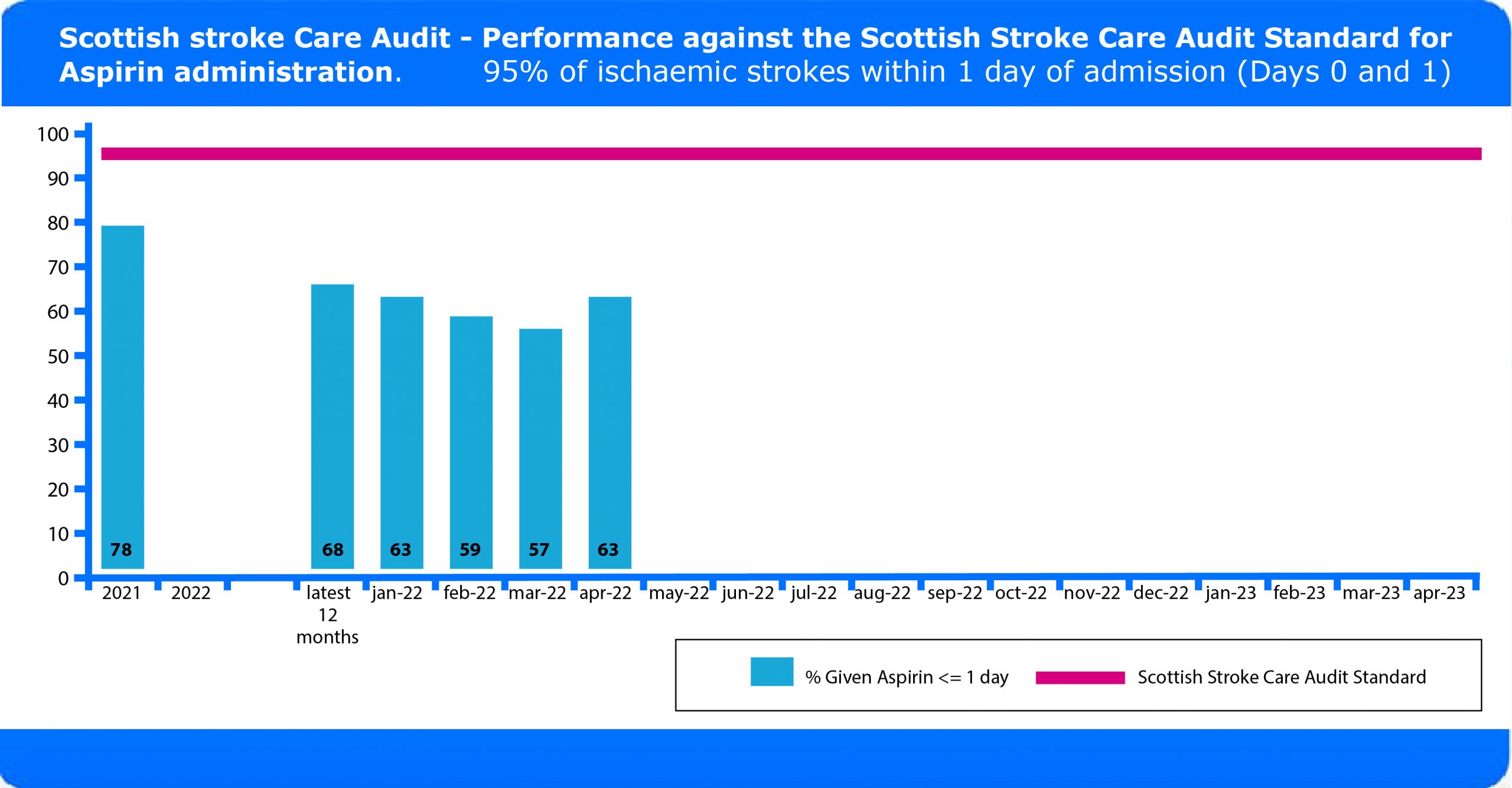
The graph below shows the results produced in April 2022 from the Scottish Stroke Care Audit. NHS Boards receive monthly reports to monitor performance against standards and where needed instigate changes that ensure the highest quality care is given to patients.
You can see from this graph that the target of 95% of patients receiving aspirin is not currently being achieved in this Health Board. (see the Clinical audit and Clinical standards topic loops below for further information).
The graph below shows the results produced from the Scottish Stroke Care Audit.
Topic Loops:
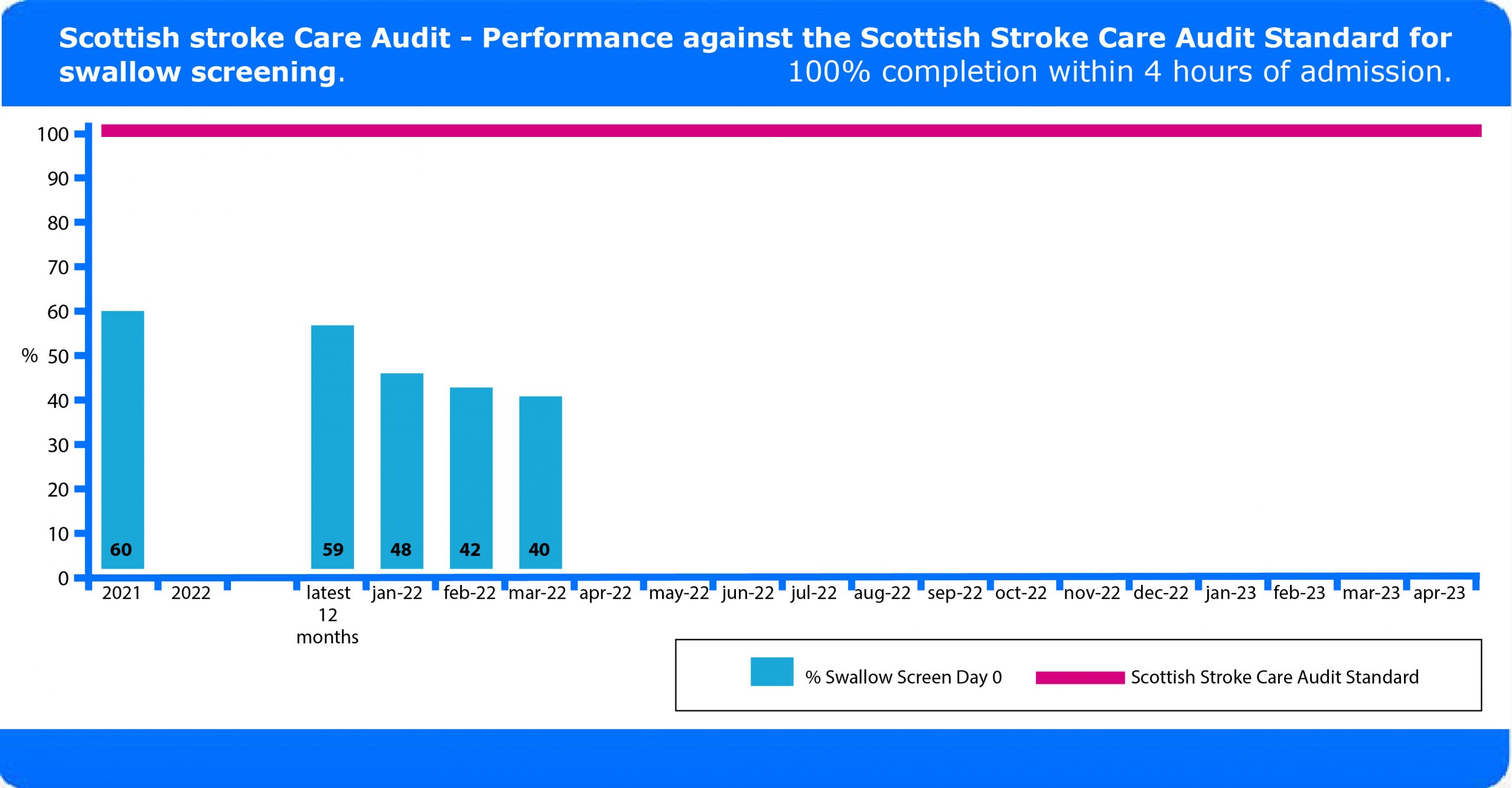 You can see from this graph that the target of 100% of patients having a swallow screen is not currently being achieved in this Health Board. (See ‘Clinical audit’ topic loop at the bottom of this page for further information.)
You can see from this graph that the target of 100% of patients having a swallow screen is not currently being achieved in this Health Board. (See ‘Clinical audit’ topic loop at the bottom of this page for further information.)
 Thomas is a 43 year old builder who self presented at the A&E department of his local hospital. He arrived at 7.30am having woken that morning with right arm weakness and slurred speech. He was assessed in the A&E department and then admitted to the medical receiving unit for further investigation. The diagnosis of stroke was confirmed by a CT scan which showed an infarct, he remained in the medical receiving unit and was transferred to the stroke unit the following day.
Thomas is a 43 year old builder who self presented at the A&E department of his local hospital. He arrived at 7.30am having woken that morning with right arm weakness and slurred speech. He was assessed in the A&E department and then admitted to the medical receiving unit for further investigation. The diagnosis of stroke was confirmed by a CT scan which showed an infarct, he remained in the medical receiving unit and was transferred to the stroke unit the following day.