Aim
To increase knowledge and understanding of the effects of multiple conditions on cardiac disease and on the management of cardiac disease.
After completing the module, you will be able to:
- Recognise the unique contribution of the Multidisciplinary Team in optimising person centred care for patients with cardiac disease and additional morbidities, regardless of individual patient profile and/or care context
- Discuss common clinical conditions that may impact on cardiac disease and its management
- Detail medications commonly used in cardiac disease and their potential interactions with those used for co-morbidities
- Discuss risk assessment and management in relation to multi-morbidities and polypharmacy
- Describe the possible psychological impact of living with multi-morbidities
- Explore integrated, person centred approaches to health and social care that may be applied in the management of patients with multi-morbidities

Module Team
Group Members
Lindsay McKechnie, Dietetic Clinical Team Lead, NHS Greater Glasgow and Clyde
Morag Osborne, Consultant Clinical Psychologist, NHS Greater Glasgow and Clyde
Irene Gardiner, Heart Failure Support Services, Chest Heart & Stroke Scotland
Betty Graham, Heart Failure Specialist Nurse, NHS Highland
Trish McDonald, Diabetes Specialist Nurse, NHS Grampian
Reviewers
Janet Reid, lead Heart Failure Nurse, NHS Lothian
Professor Allan Struthers, Professor of Cardiovascular Medicine, NHS Tayside
Learning outcomes
- Recognise the unique contribution of the Multidisciplinary Team in optimising person centred care for patients with cardiac disease and additional morbidities, regardless of individual patient profile and/or care context
- Discuss common clinical conditions that may impact on cardiac disease and its management
- Detail medications commonly used in cardiac disease and their potential interactions with those used for co-morbidities
- Discuss risk assessment and management in relation to multi-morbidities and polypharmacy
- Describe the possible psychological impact of living with multi-morbidities
- Explore integrated, person centred approaches to health and social care that may be applied in the management of patients with multi-morbidities
General Medical Disclaimer: The information, including but not limited to, text, graphics, images, recommendations, opinions and other material contained on or accessed through this website (or in any module or content accessible through this website) (together “Website”), is intended for general informational purposes only. The information should not be considered as professional medical advice, diagnosis, recommendations or treatment. The information on this Website is provided without any assurance, representations or warranties, express or implied. We do not warrant that the information on this Website is applicable to all healthcare practices, geographical locations, health needs or circumstances. We do not warrant that the information on this module is complete, true, accurate, up-to-date, or non-misleading. You should always seek the guidance of a qualified healthcare professional before making any decisions related to your health or wellbeing. Never disregard or delay seeking medical advice due to something you have read on this Website. The use of or any reliance placed on any information provided on or accessed through this Website is solely at your own risk. If you have any specific questions or concerns about your health, please consult a qualified healthcare provider or other qualified medical professional. Do not rely on the information on this Website as an alternative to medical advice from your doctor or other qualified professional healthcare professional or healthcare provider.

This is the module test for ‘HEARTe 12. Psychological impact of cardiac disease’. It is strongly recommended that you work through the learning materials of the module prior to commencing this test. By going straight to the test you may miss out on valuable learning contained within the module. The answers to all the test questions are contained within the module. This information may have been provided in the ‘Additional Information’ boxes on some of the pages.
There are 10 questions and you must answer all of these correctly to obtain a certificate of completion.
You should allow approximately 10 minutes to complete the test.
Sheila’s depressed mood has improved. She is continuing with her exercise programme and is feeling the benefits of it. Sheila and her daughter have enjoyed working on her online CBT course together and have decided to continue working on it in this way, rather than Sheila doing it on her own. The support of the SPIRIT practitioner gas been very helpful. The befriending service has provided someone to drive Sheila to and from her choir practices and sit with her husband while she enjoys an afternoon singing with her friends.
The heart failure nurse visits Sheila at home. She re-assesses Sheila using the PHQ-9 and Sheila’s score is unchanged.
The heart failure nurse has training in Motivational Interviewing and she uses this approach when chatting with Sheila about her depression.
You have been introduced to the concept of motivational interviewing in the previous case study (Angus) but, if you are interested in learning more, a number of online learning modules are available:
Medication

One of Sheila’s expressed problems is that she has difficulty remembering to take her medication. It is important to be aware of potential cognitive changes which may impact on self-management and medication / therapy adherence as there is some evidence that there may be an increased risk of experiencing cognitive changes with cardiac disease.The nurse used a validated tool, The General Practitioner Assessment of Cognition (GPCOG) to assess Sheila’s level of cognition. The tool indicates that Sheila does not have significant cognitive impairment, apart from her inability to manage her medication effectively. (There are a number of validated tools that can be used in this situation – please see below.)
The heart failure nurse contacts the pharmacist and arranges for Sheila’s medications to be prescribed in dosette boxes. Dosette boxes are individualised boxes containing medications organised into compartments by day and time. These are especially useful in patients with polypharmacy, such as Sheila. Sheila finds these much easier to use and no longer worries that she has forgotten to take her tablets.
Pulse point
Cognition
It is important that Sheila continues to be monitored for cognitive deficits, as there is a possibility that her mood might improve with treatment but her memory impairment will continue. Problems with memory, confusion, language, thinking or judgement may be due to Sheila’s depression or may be indicative of something else, for, example hypoxic brain injury. Cognitive Impairment can cause poor self-management and adherence to medication, and is associated with a worse prognosis. It also includes an increased risk of mortality in heart failure.
The following resource contains information on assessment of cognitive abilities:
The GP refers Sheila to the Cardiac Rehabilitation team.
Following her referral, Sheila’s case is discussed by the cardiac rehabilitation team. Given her difficulties in attending external appointments, the community cardiac physiotherapist telephones Sheila and arranges to visit her in her home.
For more on Cardiac Rehabilitation see the Cardiac Rehabilitation module.
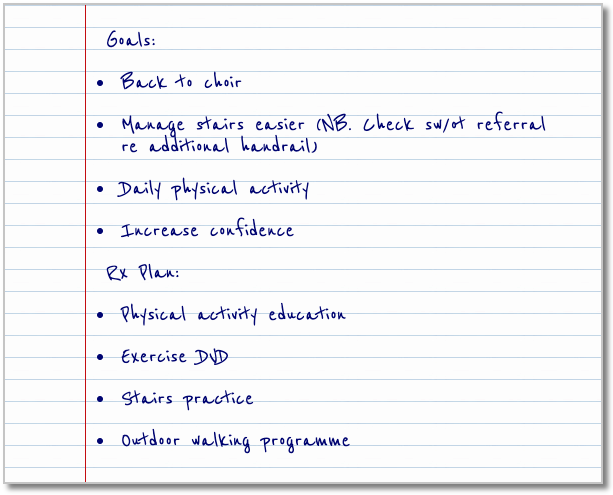
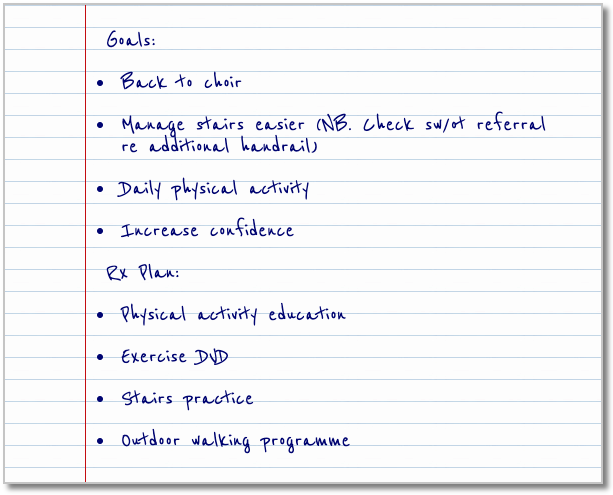
The physiotherapist reassesses Sheila using the PHQ-9: her score is unchanged from previously. He decides to use a Decisional Balance Box tool to help Sheila to think about the benefits and drawbacks of starting a structured exercise programme.
| Decisional balance |
Benefits |
Drawbacks |
| Change |
- able to return to choir practice
- able to meet with friends
- allow her to leave the house
- feel better emotionally
- feel healthier physically
|
- worry about getting too breathless
- worry about getting too tired
- if go out, husband will be left alone
|
| No Change |
- won’t worry about getting too breathless
- won’t worry about getting too tired
- won’t worry about husband being left alone
|
- won’t feel better emotionally
- won’t feel better physically
- will continue to feel lonely
- won’t be able to leave the house
|
Sheila attends for an appointment with a cardiac psychologist and, together, they agree that cognitive behavioural therapy (CBT) might help her adjust to the impact of her heart failure and develop strategies to cope with her illness. Research has shown that CBT can help improve symptoms of depression.
CBT is a form of psychotherapy that focuses on teaching people skills to assist them to see their situation in a more helpful way and to learn some skills of managing life in a more productive manner. This means it is very helpful for people who have had a cardiac event or have a cardiac disease. Having heart failure can be stressful and can make people question their ability to live with the lifestyle changes the disease can bring. CBT helps people refocus on the positive view and develop strategies for the challenges they are facing. The skills allow people to relax more, see the future in a more helpful manner and, generally, feel more in control of their life.
Please see the following videos for more information on CBT:
Although this is a resource for patients, it is a useful introduction to CBT
This video offers an indication of what happens at an initial face to face CBT session.
Sheila will find it difficult travelling to attend her local cardiac psychology department for CBT sessions, due to her breathlessness and caring for her husband, so she and the cardiac psychologist decide that she will access an online CBT course (Living Life to the Full) and that she will be supported by a practitioner trained in SPIRIT (Structured Psychosocial Interventions in Teams course Five areas: SPIRIT Training Project (Glasgow) . Sheila’s daughter has already bought her a mobile tablet to help with online shopping, and agrees to help her mother accessing the online materials until she feels comfortable doing it herself. The SPIRIT practitioner will phone Sheila regularly to support her.
The GP discusses Sheila’s depression with her and they agree on the following actions:
- referral to the Cardiac Psychology team
- referral to the Cardiac Rehabilitation team
- Sheila to be prescribed antidepressants
- Sheila to be visited at home by the heart failure nurse
Studies have shown that combination treatment of depression is more successful that treating with a single interventions, such as CBT alone or antidepressants on their own (UpToDate: Patient education: Depression treatment options for adults (Beyond the Basics))
Please enable JavaScript in your browser to see this interactive content.
Now that Sheila has been diagnosed with depression, it is important to understand why she is feeling this way. When we are thinking about Sheila’s mood the diagram below can be a helpful way of conceptualising how she is feeling and of guiding interventions to manage her depression.
Please enable JavaScript in your browser to see this interactive content.
One of the major causes of Sheila’s depression appears to be the loneliness she is feeling as her heart failure progressively affects her lifestyle. (Interestingly, research studies suggest that loneliness can be a risk factor for heart disease but it is difficult to find similarly validated research looking at heart disease as a risk factor for loneliness.)
The following articles include interesting information on loneliness:
Age UK define social isolation as “separation from social or familial contact, community involvement or access to services, while loneliness can be understood as an individual’s personal, subjective sense of lacking these things.” Loneliness has become such a major factor affecting the wellbeing of so many older people that a national campaign has been started to address this.
Sheila is feeling lonely and socially isolated because she is less able to get out of the house to socialise with people. This is partially due to her inability to mobilise as well as she previously did, due to her progressing heart failure, and partly due to her husband’s increasing dependence on her. The GP decides to ask the heart failure nurse to pay Sheila a visit, to assess whether anything can be done to combat her loneliness.