Kirsten discovers she is pregnant

Kirsten fails to attend her follow up appointments. Two years later she phones the nurse specialist and informs her that she is pregnant. The pregnancy was not planned and she has not had any recent echo or MRI scans since her surgery. The nurse specialist arranges an appointment for Kirsten at a joint cardiac and obstetric clinic. This is run by a consultant cardiologist in CHD, a consultant obstetrician and a cardiac CHD nurse specialist. They review Kirsten with a repeat echo at 14 weeks gestation. Kirsten’s pulmonary valve and right ventricle are working well. She has experienced some palpitations that last for a few minutes but she does not get dizzy, or experience breathlessness or chest pain. The nurse specialist arranges a 24hr tape for Kirsten and makes arrangements for her to be followed up both by her local team and at least once more in the clinic with a repeat echo scan. Kirsten’s case is discussed at a cardiac obstetric multidisciplinary team meeting and a care plan is developed.
Cardiac Obstetric Care Plan: Kirsten Campbell: 1234567890: 32weeks
| Diagnosis |
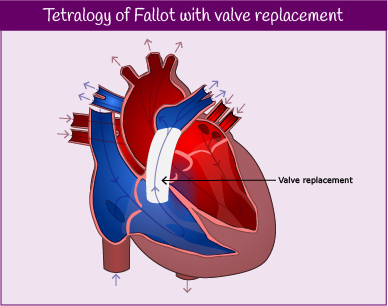
- Tetralogy of Fallot
- Moderate right ventricular dilation
|
| Prev intervention |
- Repair to Tetralogy of Fallot 1987
- Pulmonary Valve Replacement 2013
|
| Current meds |
|
| Obs history |
|
| Examination (15/01/15) |
- 60bpm & regular BP 123/64mmHg
- No significant heave or thrill
- HS I and II ESM in pulmonary region
- Chest clear, no peripheral oedema
|
| Investigations |
- ECHO (12/01/15)
- Moderately dilated RV with preserved function
- Normal LV dimensions
- RVSP 25mmHG RAP
- Peak velocity across PV 2.8m/s
- ECG (2013)
- Sinus rhythm
- RBBB
- QRS 146ms
- CPET (2013)
- Maximal test
- Good BP and HR response without desaturation
- Normal spirometry
- VE/VCO2 slope 26
- Peak VO2 80% predicted
- CMRI (Oct 2014)
- Moderately dilated RV
- Good RV dysfunction
- Good LV function and normal size
|
| Delivery Plan |
Location: Local General Hospital
- Aim for spontaneous labour, vaginal delivery
- Early epidural
- Priority to optimise analgesia
- Invasive monitoring not indicated
- No restrictions to length of second stage
If concerns from cardiology perspective contact on-call Cardiologist at SGH. |
| Post Partum Care |
- No routine requirement for obstetric HDU
|
| Follow Up |
|

Kirsten attends for surgery a few months later. She is discharged home after 7 days in hospital. Following her surgery Kirsten is reviewed by the surgeons and then receives a further assessment with her CHD team around 4 months after her operation. She has an echo and ECG performed and these are reviewed by her Consultant and nurse specialist. The function and size of her right ventricle has improved and her symptoms are much better.
Kirsten’s care is then shared between her local cardiologist and the specialist centre, who arrange to see her back at clinic in a year for a repeat assessment including MRI, CPET, echo and ECG. Kirsten knows she can contact her nurse specialist at any time, if she needs to, or if anything changes. She is made aware of the need to reduce her risk of endocarditis and also of informing the team if she plans to get pregnant in the future. This will ensure she is able to have a full assessment prior to any pregnancy.
Pulse point
Patients who have had a conduit replacement or a previous pulmonary valve replacement can potentially have future valve replacements done using a transcatheter approach. A valve is sutured within a metal stent and is delivered from the femoral vein to the heart using a balloon catheter. The procedure is less invasive and takes place under a general anaesthetic in a cardiac catheterisation lab. The hospital stay and recovery period for patients who have this procedure is often much shorter compared to patients who have cardiac surgery. For more information on transcatheter valve replacements visit Medtronic Melody: Transcatheter Pulmonary Valve (TPV) Therapy.

Kirsten’s case is discussed at a multidisciplinary team meeting. Present are a consultant cardiologist in Adult Congenital Heart Disease (ACHD), consultant cardiac surgeons specialising in CHD, ACHD nurse specialists, a cardiothoracic anaesthetist, paediatric consultant cardiologists, and sonographers.
The team review Kirsten’s case and look at her recent test results and images. Because Kirsten had symptomatic changes, functional deterioration on her cardiopulmonary exercise test and an increase in the size of her ventricle, the team decide that the timing is right to proceed with a pulmonary valve replacement.
Right Ventricle to Pulmonary Artery valved conduit
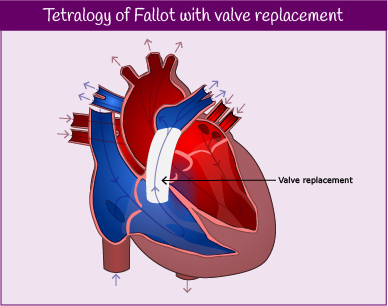
In patients with ToF, reparative surgery can either involve widening the native right ventricular outflow tract (RVOT) or, in severe cases where this is not amenable, a valved conduit can be inserted. This involves a prosthetic tube and valve being placed between the right ventricle and the pulmonary artery. This replaces the native RVOT.
Two years later, Kirsten attends her first appointment at the Scottish Adult Congenital Cardiac Service for a full assessment and review. The doctor reviews Kirsten’s ECG, exercise test (CPET), echo and MRI scan. Her exercise test shows a decrease in her exercise capacity since she was last reviewed and her echo demonstrates that her right ventricle had increased in size, due to the pulmonary regurgitation, and is now severely dilated, with some mild right ventricular dysfunction. Kirsten reports that she has been feeling more breathless during the last few months and is occasionally troubled with palpitations.
The doctor explains to Kirsten that she might need surgery on her pulmonary valve but that, in the first instance, her case will be discussed at a multidisciplinary team meeting.
Kirsten attends an appointment with the nurse specialist. The nurse gives Kirsten the contact details of the members of the nurse specialist team, before discussing a number of issues with her.
Please enable JavaScript in your browser to see this interactive content.
The nurse specialist also signposts Kirsten to the following support resources:
Please enable JavaScript in your browser to see this interactive content.
During the consultation, the consultant reviews Kirsten’s ECG and echo. The results are unchanged from her previous scans.
The Consultant asks Kirsten if she is experiencing symptoms such as palpitations, arrhythmias, chest pain or increasing shortness of breath. Kirsten denies any symptoms.
The doctor then arranges for Kirsten to meet with the nurse specialist.


Kirsten is now 16 years old and today is her first appointment at the teenage clinic, before her care is transferred to the adult service. She meets with a cardiologist from the adult service and a nurse specialist.
Kirsten remains under the care of the children’s hospital once she goes home and attends the paediatric clinic for regular reviews. She lives a normal life, attending school and taking part in usual childhood activities with her friends.
Meet Kirsten…
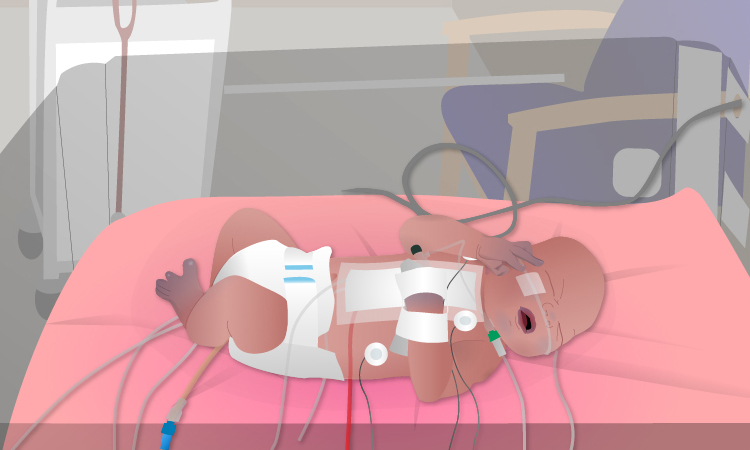
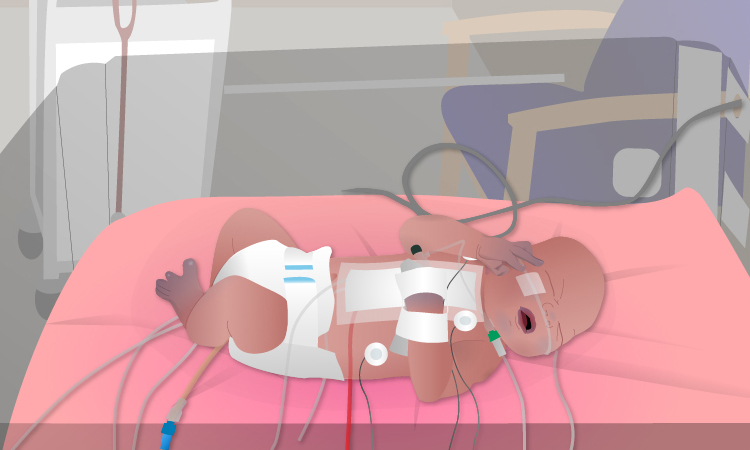
Katie’s labour is induced at 39 weeks and Kirsten is born in a hospital with specialist paediatric cardiac services. Kirsten is cyanotic at birth and is admitted to the neonatal intensive care unit. A continuous infusion of Prostin (see Additional Information) is instigated. When she is 2 days old, she undergoes palliative surgery and an aortopulmonary shunt is created.
Kirsten makes an uneventful recovery from surgery and is discharged home after ten days.
Katie and her partner meet with the consultant obstetrician to discuss the care that Katie will be offered during the remainder of her pregnancy. Katie will now be under the care of an extended multidisciplinary team:
- midwife counsellor
- consultant obstetrician (foetal medicine specialist)
- foetal/paediatric cardiologist
- paediatric cardiac liaison nurse
Please enable JavaScript in your browser to see this interactive content.