Category: HEARTe
Bill: Part 1
Meet Bill

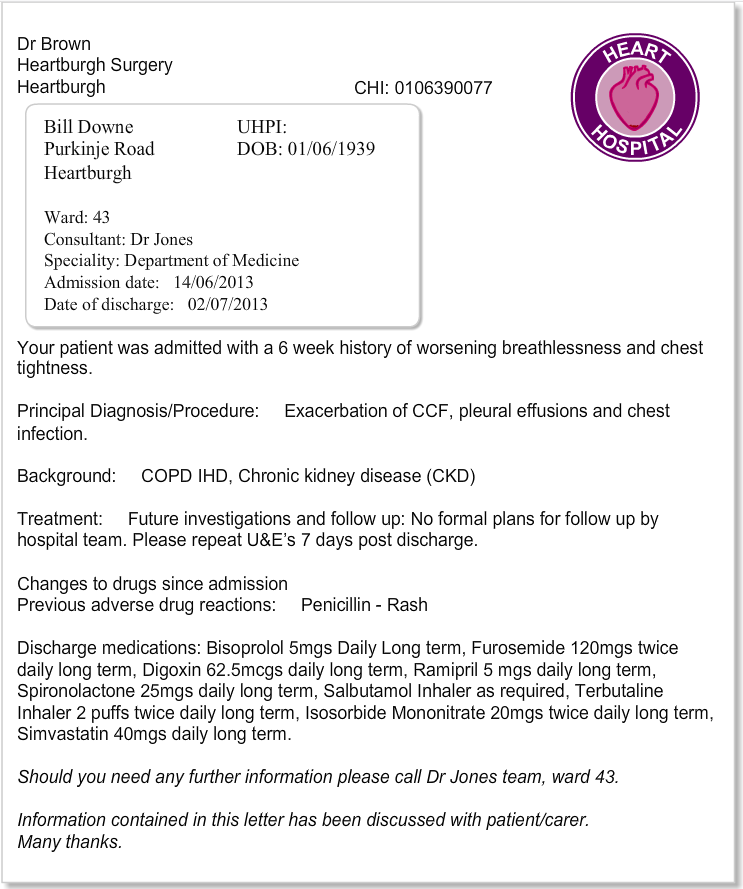
This picture introduces Bill, 3 months before his hospital admission.
Bill is a 74-year old retired teacher. He is a widow and lives alone in a one bedroom flat which has two flights of external stairs.
Bill was admitted to hospital with increasing breathlessness associated with worsening heart failure.
He was discharged after a three week stay in the medical unit.
His past medical history includes:
- Heart Failure (HF)
- Atrial Fibrillation(AF)
- Cardiovascular Disease (CVD)
- Chronic Obstructive Pulmonary Disease (COPD)
Meet Bill
![]()
Bill is a retired teacher in his 70s. He lives alone in a second-floor flat.
Throughout this module you will be able to follow Bill’s journey from hospital discharge. The module will illustrate core aspects of supportive palliative care as well as the unique contribution of the wider multi-disciplinary team particularly as Bill’s disease progresses and his needs escalate.
Supportive and palliative care
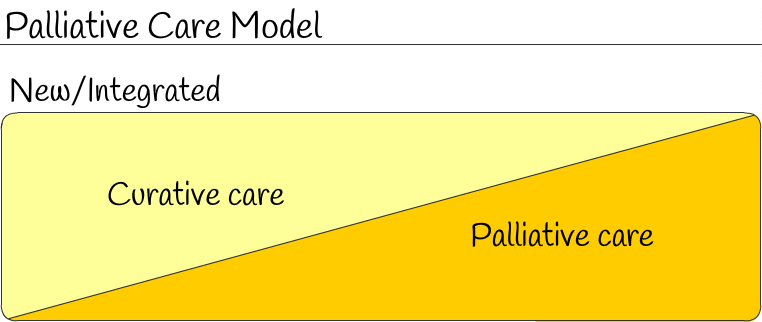
It is now recognised that many patients will benefit from a supportive and palliative care approach.The principles of supportive and palliative care are integral to the care delivered by any health or social care professional to those living with and dying from any advanced, progressive or incurable condition.
Palliative care is not just about care in the last months, days and hours of a person’s life, but about ensuring quality of life for both patients and families at every stage of the disease process from diagnosis onwards. A palliative care approach should be considered parallel to optimal cardiological treatment (See image below).
Palliative care focuses on the person, not the disease, and applies a holistic approach to meeting the physical, practical, functional, social, emotional and spiritual needs of patients and carers facing progressive illness and bereavement. (Scottish Government 2008).
“Patients with heart disease, particularly heart failure, who remain symptomatic despite optimal treatment, have physical, psychological, social and spiritual needs that may benefit from supportive and palliative care leading to improved quality of life (NHS QIS 2010)”.
New concept: It is now recognised that supportive and palliative care can be combined with disease modifying cardiac treatments.
References
NHS QIS, (2010) Clinical Standards for Heart Disease. NHS QIS, Edinburgh. Healthcare Improvement Scotland
Living and dying well: a national action plan for palliative and end of life care in Scotland: Available at : The Scottish Government
Palliative care approach
What is palliative care?

The World Health Organization (WHO) defined palliative care as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.
WHO recommended that planning for care at the end of life should be responsive to patient choice regarding place of care and place of death.
The following links relate to the delivery of palliative care within cardiac disease:
Healthcare Improvement Scotland:
Living and Dying Well:
Improvement Hub Scotland: LWIC – Palliative and End of Life Care
Learning outcomes

Identify an awareness of triggers that may suggest a declining change in the person’s overall condition.
Review the evidence available to support the holistic assessment influencing the delivery of supportive palliative care for persons living with and dying from advancing cardiac disease.
Recognise the unique contribution of the Multi Disciplinary Team (MDT) in optimising person-centred care.
Introduction

Module authors
Module lead
Yvonne Millerick Lead Nurse Lecturer for the Heart Failure Palliative Care “Caring Together” Programme, a partnership between NHS, GG&C, BHF, MCCC and Glasgow Caledonian University
Module authors
Dr Karen Hogg, Consultant Cardiologist NHS GG&C & Caring Together Programme, NHS Greater Glasgow & Clyde
Andrea Ness, Heart Failure Specialist Nurse, NHS Lothian
Betty Graham, Heart Failure Specialist Nurse, NHS Highland
Jacquie Lindsay, Palliative Care Nurse Lecturer, St Margaret of Scotland Hospice, Glasgow
Reviewers
Julie Churchill, Long Term Condition Community Nurse, NHS Lothian
Gordon Macleod, Community Unscheduled Care Nurse, NHS Western Isles
Dr Leslie Cruikshank, Clinical Lead, Falkirk CHP
Contributors
Sandra Campbell, Nurse Consultant, Cancer & Palliative Care, NHS Forth Valley
7. Palliative care
Learning outcomes
- Identify an awareness of triggers that may suggest a declining change in the persons overall condition.
- Review the evidence available to support the holistic assessment influencing the delivery of supportive palliative care for persons living and dying from advancing cardiac disease.
- Recognise the unique contribution of the Multi Disciplinary Team (MDT) in optimising person centred care.
General Medical Disclaimer: The information, including but not limited to, text, graphics, images, recommendations, opinions and other material contained on or accessed through this website (or in any module or content accessible through this website) (together “Website”), is intended for general informational purposes only. The information should not be considered as professional medical advice, diagnosis, recommendations or treatment. The information on this Website is provided without any assurance, representations or warranties, express or implied. We do not warrant that the information on this Website is applicable to all healthcare practices, geographical locations, health needs or circumstances. We do not warrant that the information on this module is complete, true, accurate, up-to-date, or non-misleading. You should always seek the guidance of a qualified healthcare professional before making any decisions related to your health or wellbeing. Never disregard or delay seeking medical advice due to something you have read on this Website. The use of or any reliance placed on any information provided on or accessed through this Website is solely at your own risk. If you have any specific questions or concerns about your health, please consult a qualified healthcare provider or other qualified medical professional. Do not rely on the information on this Website as an alternative to medical advice from your doctor or other qualified professional healthcare professional or healthcare provider.
Key messages
By the end of this case you should understand:
- Pharmalogical treatment and non-pharmalogical treatment of acute Heart Failure (HF)
- Psychological influences in caring for patients and their carers living with HF and devices
- Develop and awareness of the benefits and support HF patients should be able to apply for


