Thrombolysis involves an injection of clot busting drugs (e.g tenecteplase), which are given directly into the vein.
Thrombolysis treatment may be an emergency treatment if PCI is not available. Treatment with thrombolysis is most effective when it is given as soon as possible. This helps to reduce damage to the myocardium and reduce the risk of complications. It may be administered by paramedics or GPs if transfer to hospital would delay treatment.
This treatment is not suitable for everyone as there is a risk of bleeding.
A standard treatment regime would be:
- Unfractionated heparin (5000 units IV)
- Tenecteplase (100 units per kilo IV)
Thrombolysis can also be given to reperfuse the brain after a stroke. For more information about thrombolysis in the treatment of stroke refer to: Stroke Training and Awareness Resources (STARs).
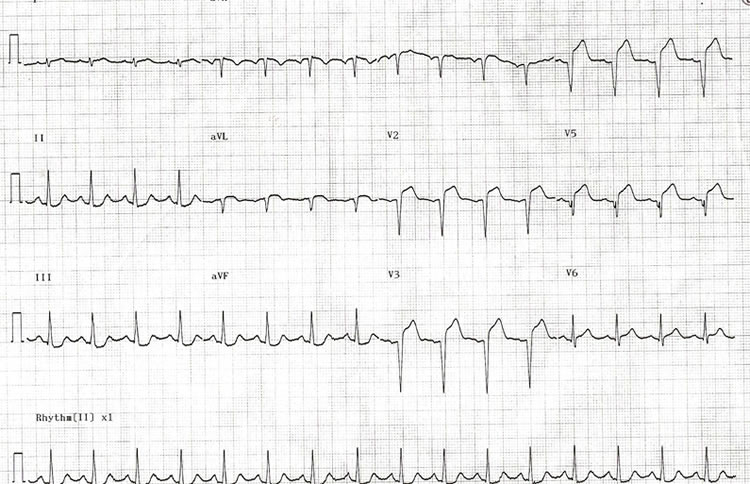
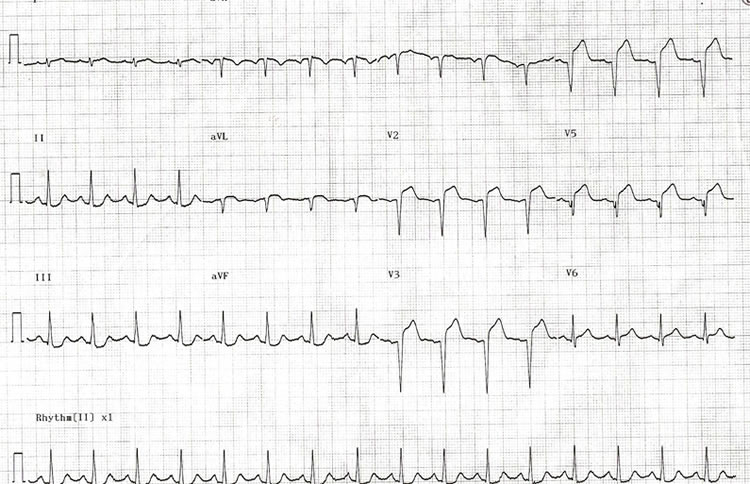
Based on initial Electrocardiogram (ECG) and clinical presentation, Joan is diagnosed with an anterior ST Elevation Myocardial Infarction (STEMI). Her case is discussed with an interventional cardiologist who feels that the time delay involved in her transfer to the interventional centre is too long for primary angioplasty. He recommends that she receives thrombolysis if there are no contraindications and transfer for assessment for Percutaneous Coronary Intervention (PCI) thereafter.
Joan is admitted to the emergency department after 5 hours crushing chest pain at rest.

 Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
After a long journey they both decide on an early night. Joan is wakened at 5am by a crushing pain in the centre of her chest. She has never experienced anything like it before, and feels short of breath and nauseated. She does not want to alarm Mark but after 2 hours she wakens him as she is no better and starting to feel very frightened. Mark notices that Joan is clammy to touch and is concerned, he wants to ring for an ambulance but Joan refuses as she does not want any fuss. Mark finds an information pack in the cottage with details of the local community hospital and Mark drives her there. Joan vomits on her arrival at the hospital.
Having completed this module the learner should;
- have an understanding of the diagnosis and management of patients who present with symptoms indicative of Acute Coronary Syndrome.
- recognise the benefits for patients and carers of utilising a holistic multidisciplinary approach to care.
- be aware of the resources available to ensure that their practice is evidence based and have knowledge of local workplace procedures and practice.
The following are all secondary prevention strategies that Hamish should be encouraged to address.
Hamish is discharged home. He has been referred to the cardiac rehabilitation service and receives a phone call from the cardiac rehabilitation nurse, Gillian.
There are several key areas that the cardiac nurse Gillian focuses on during her telephone assessment, she uses the SBAR* framework to provide structure and focus to her assessment.
Prior to surgery, Hamish will be seen by the surgeon in order to discuss the operation and potential risks and benefits. The surgeon tells him he will need a number of tests and investigations prior to the operation. In Hamish’s case this will be carried out as an in-patient. However most people follow an elective pathway for cardiac surgery and are admitted from home.
| Pre-assessment requirements for cardiac surgery |
| Assessment |
Rationale |
| Medication |
Changes may be required to medication prior to surgery according to the surgeons preference. |
| Chest X-ray (CXR) and Pulmonary Function Tests (PFT”s) |
CXR is important to identify underlying pathologies or infection prior to surgery. PFT’s are required to assess respiratory function as part of anaesthetic assessment. |
| Blood tests |
A broad range of blood tests are required prior to cardiac surgery in order to establish baseline values preoperatively. Group & Save is included in case blood transfusion is required. |
| Methicillin Resistant Staphylococcus Aureus (MRSA) Screening |
The purpose of screening for MRSA is to identify, manage and reduce risk of transmission of MRSA. Screening may include taking swabs from the nose, throat, axilla, groin or perineum. |
| Urine dipstick |
This forms part of the overall general inpatient assessment. |
| Dental Assessment |
Not a requirement for people awaitibg CABG, although a desirable part of overall good health and essential for those having valve surgery or the correction of congenital defects. |
| Other |
Additional tests may include an ultrasound of the carotid arteries to better inform the risk of stroke and echocardiogram to assess the function of the heart valves and left ventricle. |
Hamish underwent a Coronary Artery Bypass Graft (CABG) and made a good post-operative recovery. Click on Additional Information to see other aspects that may affect Hamish’s recovery.
As his coronary angiogram has shown 3-vessel disease (disease present in three different coronary arteries) Hamish is referred to the cardiothoracic team for assessment for Coronary Artery Bypass Graft (CABG) Surgery.

 Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.

