Press play on the animation below if it doesn’t start automatically for you, and then move through the slides underneath by < and >.
Category: HEARTe
Medication non-adherence
Medication non-adherence is a huge financial burden for the NHS as well as causing additional morbidity/mortality for the individual patient. Complete the following quiz to consider aspects of this.
Ben attends the practice nurse

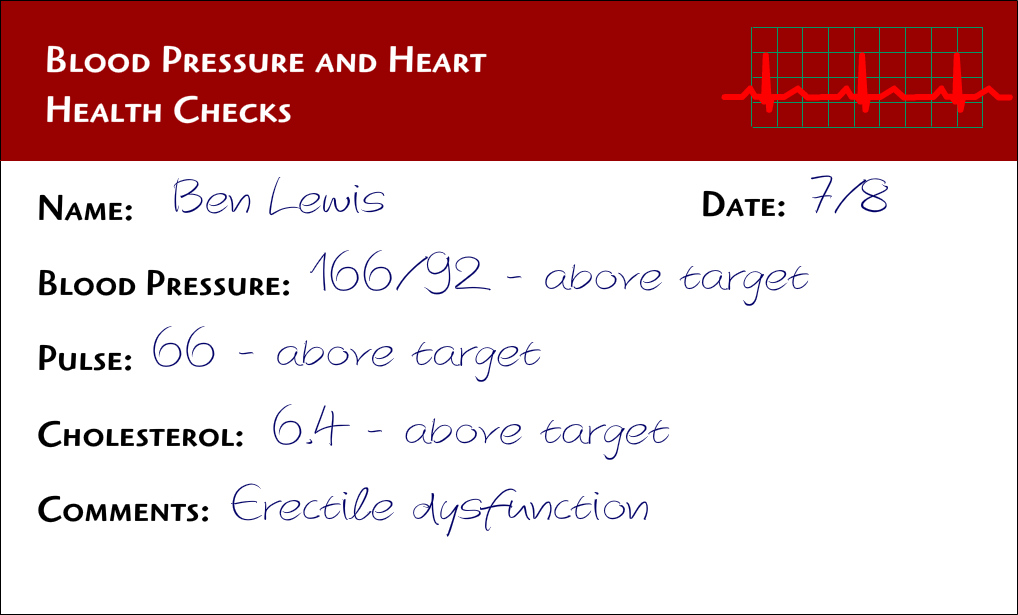
Ben goes to see the nurse the next day as the doctor has suggested she begins discussing with him the reasons he has not been taking his medications. The nurse summarises the main issues with Ben regarding his assessment and notes his readings down. She explains that target readings are decided using evidence based guidelines and are directly related to secondary prevention of further cardiac events.
Ben asks the nurse if she can be clearer about these as he doesn’t understand the jargon. The nurse then explains more about the targets for BP and cholesterol levels. She then shows Ben his results in relation to these targets. Ben says he now feels like he has a better understanding about how and why he needs assessed and how his medications are affecting these. When the nurse shows Ben the results she explains that the first three problems are all related to the fact that Ben is not taking his medications.
She tells him that any problems that have occurred since stopping his medicines are unlikely to be related to his medicines as he hasn’t been taking them. She explains that not being adherent to medications can have effects for the long term.
The GP calls Ben to discuss his test results
The GP calls Ben to discuss his test results.
Ben attends his GP
Ben plucks up the courage to go and see his GP and discusses his impotence problem but fails to mention that he is not taking all his medications. The GP takes a thorough history and examines Ben. He explains that he would like to carry out some observations and obtain some blood tests before deciding on future management of Ben’s problem.
Note: The GP observes that Ben’s BP and pulse are above target but can see how uptight Ben is during the consultant having to discuss this very difficult problem. He advises Ben that he will contact him with the results in a few days and see him back at the surgery in a couple of weeks.
Ruth and Ben’s discussion
Ruth the pharmacist considers Ben’s request
Erectile dysfunction (impotence) is commonly found in people suffering from CHD. Artherosclerosis (hardening of the arteries) affects all arterial beds throughout the body including the penile arteries (see diagram in introduction). It’s clear at the moment we don’t know what medications Ben is prescribed but review of cardiac medications is required as well as a physical/psychological assessment as some cardiac drugs are known to cause impotence and Ben has entered into a new relationship after being a widow for several years which potentially may be linked emotionally.
Ben goes to the pharmacist
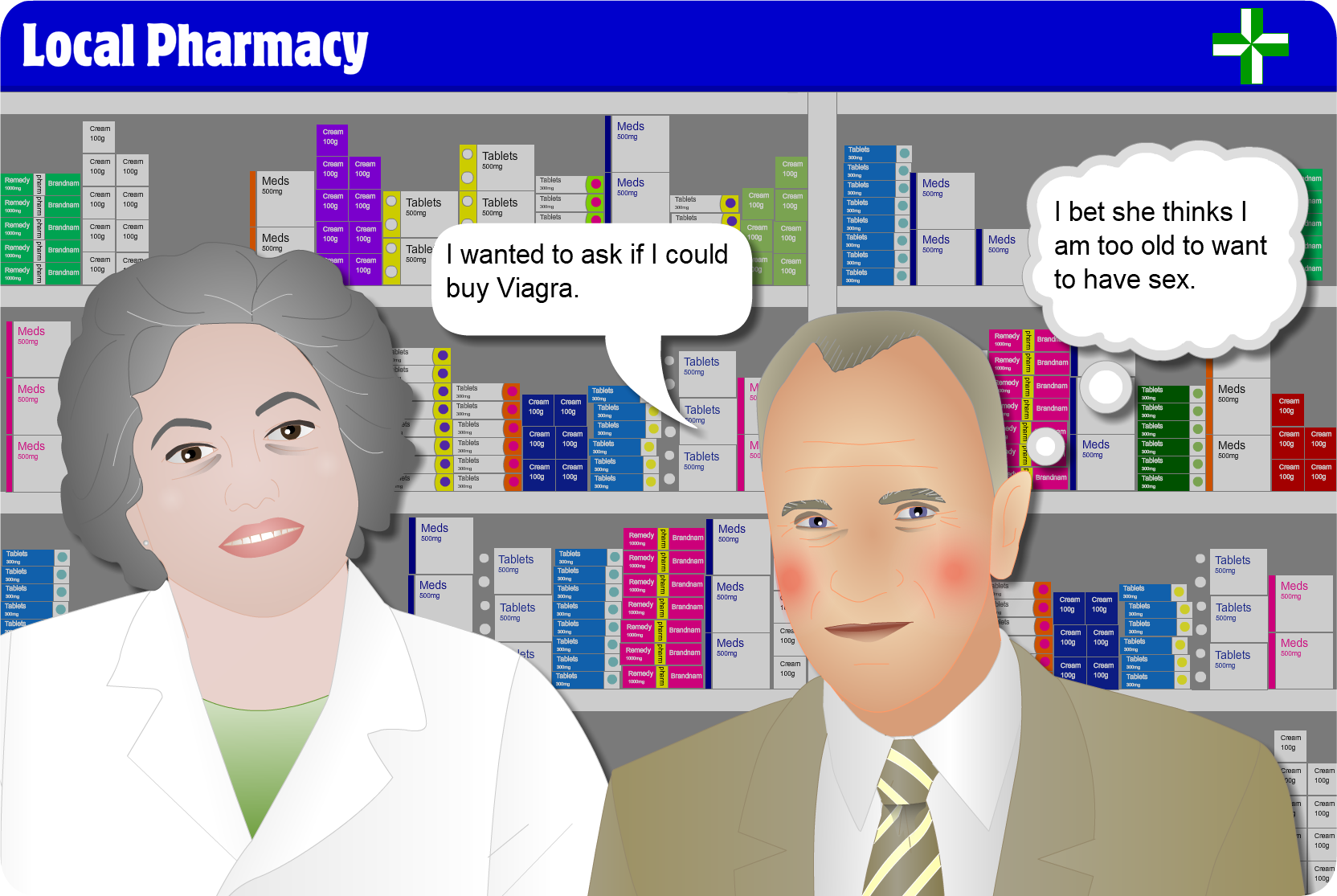
Ben speaks privately with the pharmacist. She takes him to a private consulting room and they begin talking. Ben tells her he had a PCI and stent last year and apart from this problem he says he has been feeling well but admits he has stopped some medicines he was prescribed then.
Ben
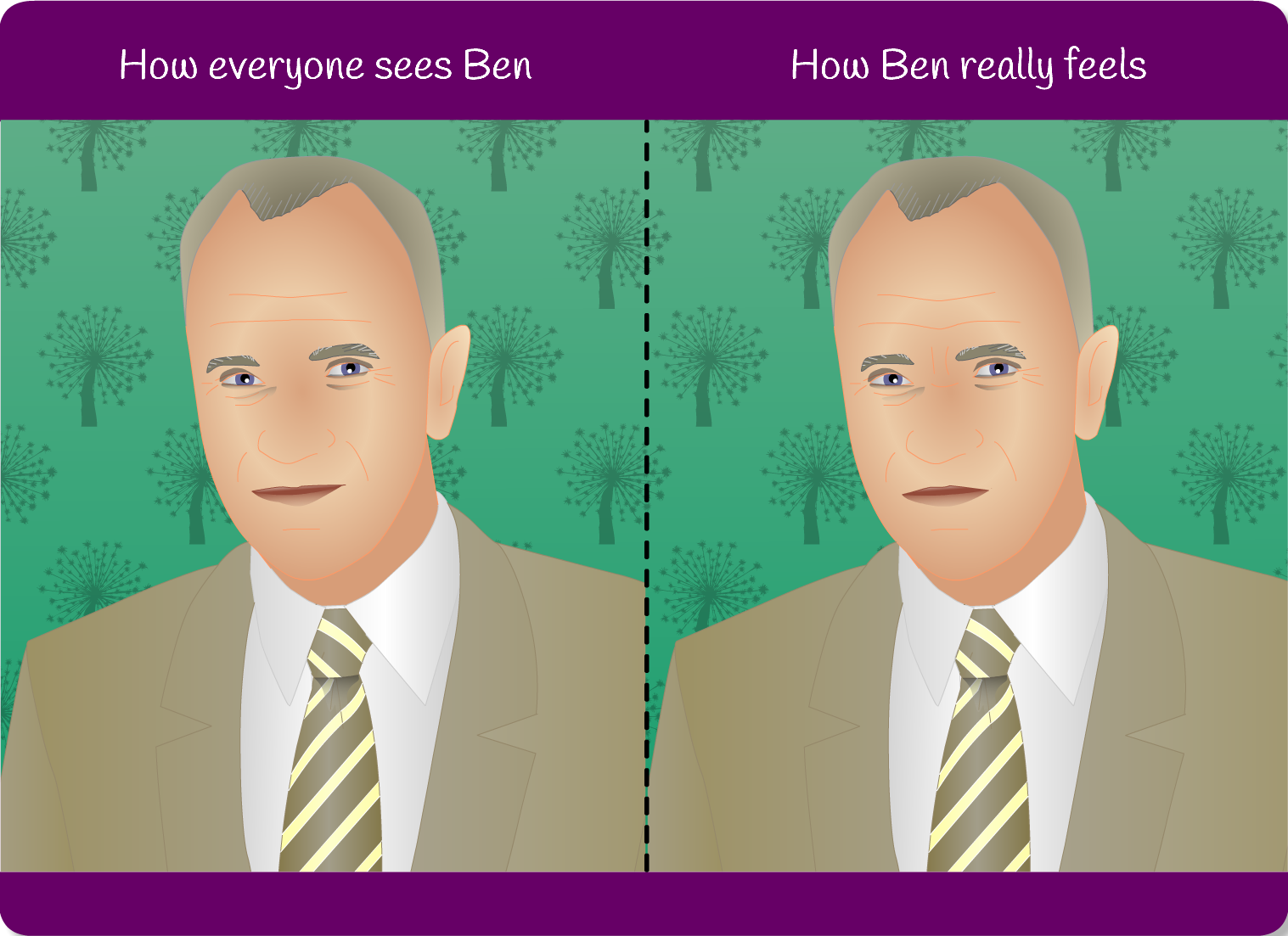
| How everyone sees Ben | How Ben really feels |
|---|---|
| Ben is a fit gentleman who has has a percutaneous coronary intervention (PCI) a year ago and has no other relevant past medical history.
Ben lost his wife 5 years ago and has been attending a local dance group where he has met Senga, a 60 year old lady. |
Ben has had a recent problem with erectile dysfunction which he finds very difficult to discuss, He has recently attempted to have intercourse with his new partner but this has failed on several occasions. He has heard about viagra and decides to ask the chemist. |
Key messages
- Clinical history – taking the time to take a focused clinical history is key to making a diagnosis and reducing the risk of missing the possibility of a cardiac cause which could have life-threatening consequences.
- Referral to Rapid Access Chest Pain (RACP) is vital for patients with a suspected new diagnosis of Angina or where there has been a change to previously stable symptoms (Bear in mind that if this is a sudden change and ACS is suspected, this warrants emergency admission to hospital). This allows a focused clinical history and cardiovascular assessment to take place, as well as further investigation by ETT if appropriate.
- Risk Factors – It is important to investigate the patients past medical history and risk factors for CHD so that opportunities for lifestyle change and intervention (such as stress management) can be put in place to reduce risk.
- Exercise Tolerance Test – a positive exercise tolerance test along with a history suggestive of Angina lends weight to the diagnosis however the angiogram is really the gold standard test which is required to demonstrate evidence of coronary artery narrowing.
- Action if further chest pain – whilst awaiting angiography it is important to ensure that the patient has a clear understanding of what action to take if she experiences any chest pain and in particular if this pain does not respond quickly to rest or GTN, namely that she must call 999.


