- Confirm trial of alternative or clinically assisted nutrition and hydration
- Feedback reports on progress from MDT – with limited engagement in rehab
- Ask if they have been able to be involved in any therapy sessions and what they thought
- Share that at such times families often think about conversations they have had together that can give a clue to what they would want us to do in this situation – allow time to respond
- Detail likely extent of disability and that this is likely to persist
- Refocus on what would be important to the patient
Video notes
- Starting a discussion about long-term alternative or clinically assisted nutrition and hydration. The final decision about whether or not to provide long-term alternative or clinically assisted nutrition and hydration is difficult and will be informed by patient and family priorities
- There can be variation between different patients and families about whether to provide clinically assisted nutrition to patients after stroke
- Some patients would want to continue living even if this means being severely disabled whilst others would prefer death rather than survival with severe disability.
- Note how the staff establishes the families’ understanding of the situation. Staff is open and appears interested and sympathetic.
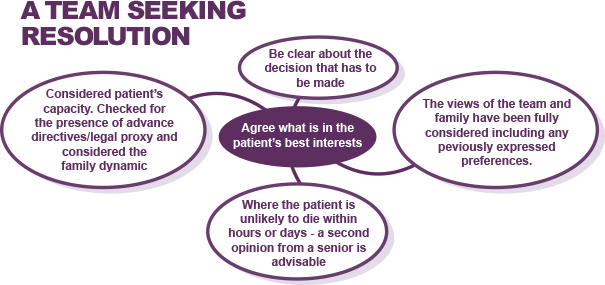
A Team Seeking Resolution
Agree what is in the patient’s best interests
- Considered patient’s capacity. Checked for the presence of advance directives/legal proxy and considered the family dynamic.
- Be clear about the decision that has to be made
- Where the patient is unlikely to die within hours or days – a second opinion from a senior is advisable
- The views of the team and family have been fully considered, including any previously expressed preferences.
Page last reviewed: 16 Jan 2023


