Animal studies have shown the following:
- Muscles immobilised in a shortened position lose sarcomeres.
- Anti-gravity and weight bearing muscles immobilised in a shortened position lose sarcomeres more quickly.
- Once sarcomeres are lost they are replaced by connective tissue. This results in a loss of muscle elasticity.
- Muscles immobilised in a neutral position maintain their sarcomeres.
- Muscles immobilised in a lengthened position gain more sarcomeres.
- Once a muscle has become shortened, if it is immobilised in a lengthened position it can regain sarcomeres.
As well as these biomechanical changes in the muscle, there can also be changes in other soft tissues such as tendons and within the joint. This makes the muscle stiffer, more resistant to passive stretch and can result in reduced joint movement.
- Muscle fibres are replaced with collagen and fatty tissue.
- Collagen proliferates into joint space, this occurs within the first 2 weeks.
- Connective tissue when immobilised forms cross bridges between collagen fibres and thus elasticity is removed = THIXOTROPHY.
- Prolonged immobilisation affects joint cartilage – it gets thinner at point of contact.
Relevance for your practice
Positioning has an impact on biomechanical changes in muscle, soft tissue and joints.
Good positioning from day one for every patient is vital in preventing these biomechanical changes.
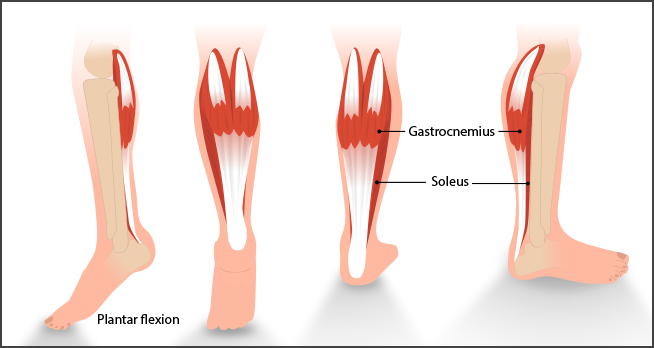
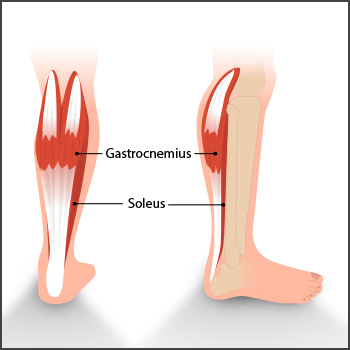
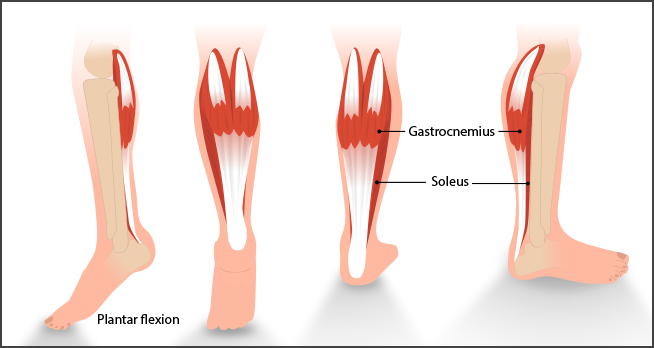
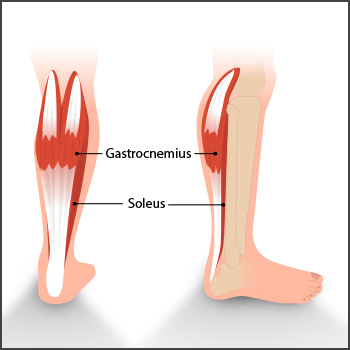
All staff should know how to correct shortened positions and make positioning part of your care plan as soon as the person is admitted to hospital after stroke. This is very relevant to staff looking after patients in bed who will be returning to weight bearing and to physiotherapists involved in early mobilisation of patients, because muscles like soleus and gastrocnemius will be more affected.
The process of muscle shortening is reversible – so proactive treatment and good positioning from day one for every patient is essential and cost effective.
These findings are directly relevant to all stages of treatment and rehab – even if you are the best nurse, physio or occupational therapist in the world you cannot achieve the best treatment or outcome available if your patient can’t get their heels on the floor or reach out to grasp because of tissue shortening.
Muscle tension is important for contraction/function:
Muscles in neutral position do not develop significant changes in stiffness or sarcomere numbers
(Gracies 2005)
At a clinical level, there are two main things to consider in relation to tone in the muscle:
- Neurogenic component: overactive muscle contraction
- Biomechanical component: stiffening and shortening of the muscle and other soft tissues due to immobility
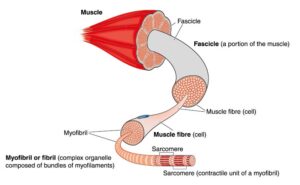
Illustration: Muscle > Muscle fibre > Sarcomere
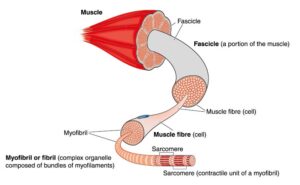
Muscles consist of contractile tissue and connective tissue. The working mechanism of contractile tissue is myosin and actin myofilaments which interlock.
Units of the contractile tissue are sarcomeres which lie in series and form myofibrils. Bundles of myofibrils form muscle fibres. These fibres are held together to form fascicles which form the entire muscle.
Connective tissue surrounds and binds each fibre. This is made up of collagen and elastic fibres.
After a stroke there may be:
- A reduction in the number of sarcomeres (atrophy)
- A decrease in overall length of sarcomeres (muscle becomes shorter)
- A relative increase in proportion of connective tissue (muscle becomes stiffer)
You need to know some neuroanatomy to understand how the brain and spinal reflexes affect the muscles. If you want to look at or revise the descending neural tracts from the brain to the spinal cord please see Additional Information for more details.
Here are the normal spinal reflexes and how a muscle contraction works. Imagine you strike the patella tendon at the knee with a tendon hammer.
Reflexes after stroke

Normal efficient movement can be affected by the following factors after a stroke:
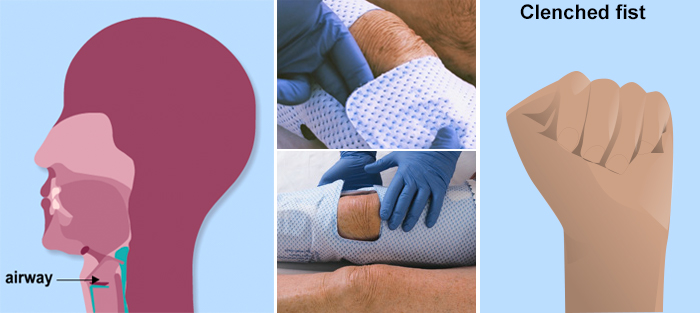
- Joint range can be impaired and muscle length shortened – hand, foot, hamstrings, Achilles tendons, shoulder movement
- Gait or walking pattern require more effort and can be uncoordinated
- Balance, normal righting reactions are slower
- Falls or fear of falling
- Functional problems, reaching, grasping objects
- Contractures
- Pain (particularly shoulder pain)
- Pressure areas at risk due to reduced mobility
- Decreased mobility
- Increased dependency
- Limb paralysis
After her stroke Sally is much slower performing functional tasks like making tea. She has to focus on balance and the position of her body in relation to the task. She may not be able to balance for long periods. Her movements require much more effort. Coordination, strength and grip have been affected. She may have difficulty opening cartons and jars. If she has muscle shortening or a contracture she may not be able to reach and grasp objects she needs. There may be sensory loss which could lead to dropping objects or risk of injury from spilling hot liquid.
An Occupational Therapy assessment along with Sally’s self management priorities and goals could help her to position her affected upper limb in stretched positions, relaxed positions or using bilateral techniques to improve both her tone and performance.
When assisting your patients during functional tasks, bear in mind the position of their limbs and use the task to move or support the limb in as normal a movement pattern as possible.

Before stroke Sally was able to make a hot drink safely, easily and quickly because she had smooth, effortless, coordinated movement, good grip strength and no sensory loss.
Normal efficient movement can be affected by the following factors after a stroke:
Sensation:
- Touch, hot and cold
- Pain, proprioception (ability to be aware of position, motion and equilibrium within the body)
- Stereognosis (the ability to recognise an object by touch alone)
- One and two point sensory discrimination (ability to recognise that two nearby objects touching the skin are truly two distinct points, not one)
Tone:
- Too high (Hypertonus)
- Too low (Hypotonus)
- Changes in tone due to position
- Associated reactions (abnormal reflex activities which may occur in the absence of voluntary movements)
- Limb position
Patterns of movement:
- No movement
- Some selective movement
- Ataxia (lack of voluntary coordination of muscle movements)
- Apraxia ( difficulty with the motor planning to perform tasks or movements when asked, provided that the request or command is understood and he/she is willing to perform the task)
Understanding movement
To understand what happens to muscles and movement after a stroke we must first look at normal movement.
Normal efficient movement is the ability to perform a movement that is:
- Smooth
- Efficient
- Co-ordinated
- Goal orientated/specific
- Graded
It may be :
- Voluntary or involuntary
- Automatic
- Following patterns
Incidence and prevalence of spasticity after stroke
-
- 38% develop spasticity
- 15% require pharmacological treatment
- 5% will require botulinum toxin injections
Verplancke D, Snape S, Salisbury CF, Jones PW, Ward AB (2005) A randomized controlled trial of botulinum toxin on lower limb spasticity following acute acquired severe brain injury. Clin Rehabil 19: 117-125.
There are some early predictive factors of long-term upper limb spasticity after stroke Part of the SALGOT study (Stroke Arm Longitudinal study at the University of Gothenburg, prospective cohort study protocol): Margit Alt Murphy, Hanna C Persson, Anna Danielsson, Jurgen Broeren, Åsa Lundgren-Nilsson and Katharina S Sunnerhagen
-
- Reduced sensorimotor function
- Spasticity at 10 days – likely at 12 months
- Spasticity at 4 weeks – severe at 12 months
- Older age – reduced probability for spasticity
Alt Murphy et al. BMC Neurology 2011, 11:56
On completion of this module you will have increased understanding of:
- Abnormal tone following stroke.
- Signs which may predict who will have tone changes and factors which may aggravate abnormal tone.
- How to identify tone changes.
- How to manage abnormal tone including knowledge of physical and pharmacological interventions.
- How individuals can self manage to prevent symptoms or further complications.
- When to refer to specialist spasticity services.
We all need to be able to tense and relax our muscles in a smooth, coordinated way in order to move and function normally. This constant flux in the levels of muscle contraction (tone) as we move and rest is usually subconscious and occurs automatically as we go about our daily lives. Following damage to the brain, such as after a stroke, we commonly see alterations in the usual patterns of muscle tone which make movement and function difficult. As a result muscle tone may become too high or too low to move normally.
All stroke patients have the potential to develop muscle tone management issues, regardless of the size or location of the stroke. Around 40% of stroke patients exhibit spasticity on discharge from hospital. (Ref) The extent of this problem can be influenced by the quality of care and therapy patients receive during their recovery. Muscle tone that is not well managed may have negative effects on physical and functional outcomes. Rehabilitation aims to address these difficulties. Everyone who works with a stroke patient in the course of their recovery, in hospital or at home can positively influence outcome with respect to tone management.
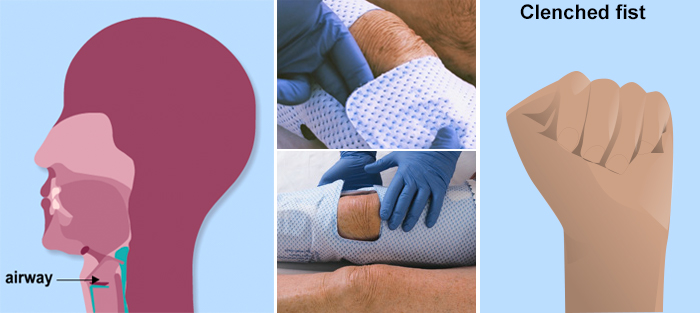
Until recently, the management of muscle tone after stroke had been less of an explicit priority in the national stroke strategy than other post stroke risks such as pneumonia, dysphagia (through disordered swallow) and DVT (through immobility and failure to adequately fit intermittent compression sleeves) for example. As a result, a section on tone management is now specifically included within the Scottish Stroke Improvement Plan (Ref) and this module is designed to empower clinicians to manage patients well with respect to muscle tone issues after stroke. In future, the extent of tone management service provision in Scotland will be audited across health board sites.
The specific aims of this module are to explore the clinical presentations of abnormal muscle tone, gain understanding of its nature, causes and solutions from physical, functional, medical and psychological perspectives. The impact and implications of tone management will be considered with respect to individual case scenarios, service delivery, clinical pathways and health economics. Best evidence will be presented to support the recommendations made within this module. The reader will be able to engage with a range of interactive tools for learning and will have the opportunity to validate that learning through a test at the end of the module.