Angela has received the bolus of Alteplase and the infusion is running. She is transferred to the acute stroke unit for monitoring.
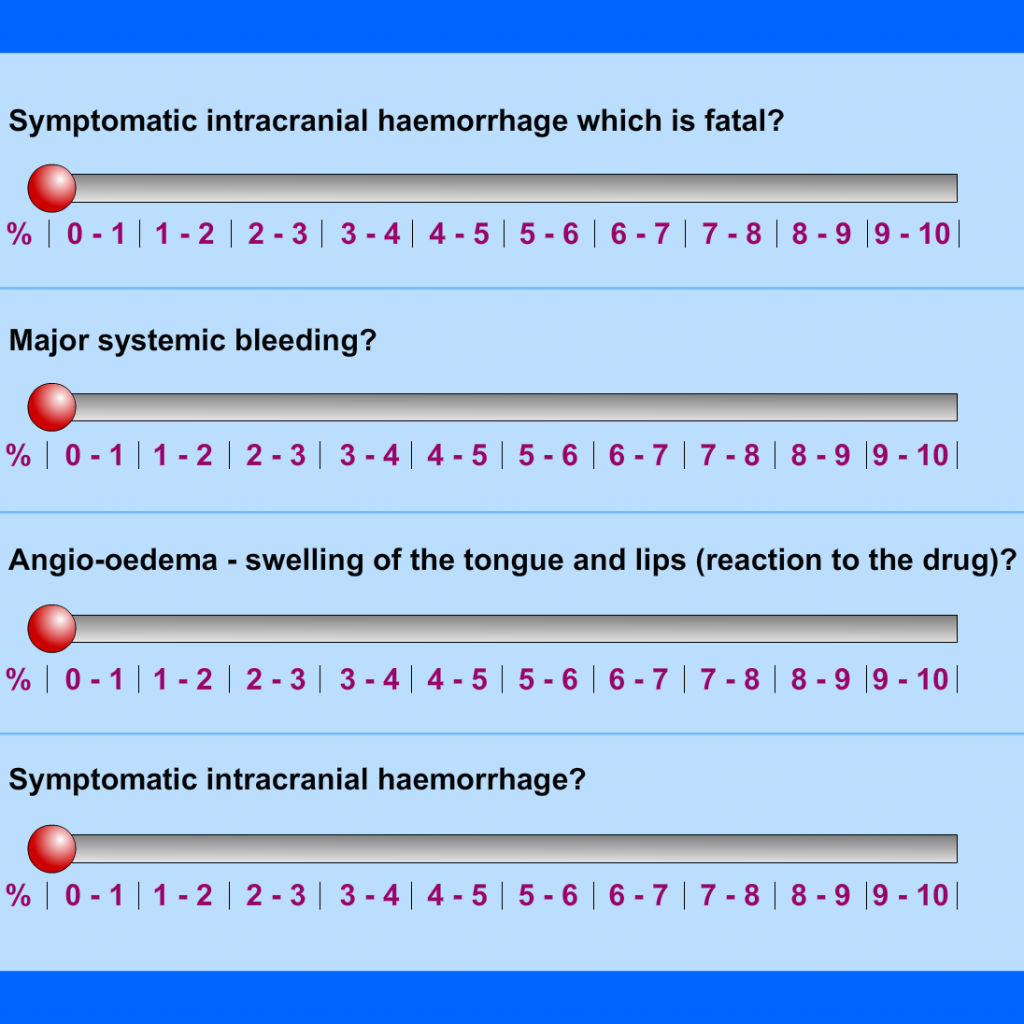
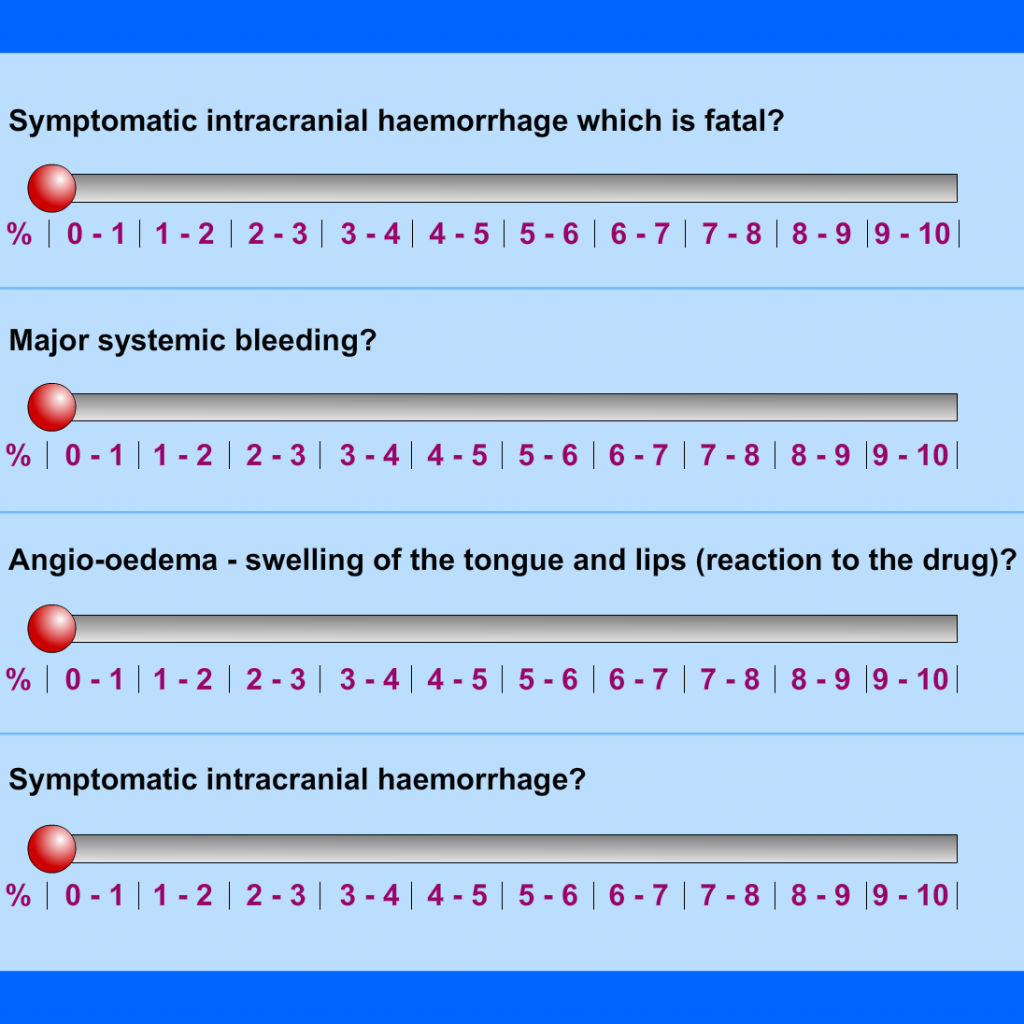
Listed below are a number of potential things that might happen after a stroke patient has been thrombolysed. How frequently do you believe each occurs? Find the correct %.
References:
Michael D Hill, Alastair M Buchan 2005. Thrombolysis for acute ischaemic stroke: results of the Canadian alteplase for stroke effectiveness study. Canadian Medical Association Journal 172 (10) 1307-1312
Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke Monitoring Study (SITS MOST): An Abbreviated Study. The Lancet, Vol 369 Jan 27 2007 275-282
Clinically assisted nutrition and hydration are treatments and therefore can be stopped or started according to clinical assessment of benefit. These decisions are likely to be emotional for those involved and are likely to raise some difficult questions. These need to be carefully considered and fears supported to avoid any potential feelings of guilt emerging.

All patients and families should have thrombolysis treatment explained clearly to them, including the benefits and risks.
Start with a brief explanation of what has happened – a stroke due to a blocked blood vessel.
Then explain that brain cells are being damaged – but that if we can unblock the blood vessel we may reduce the amount of damage. This can lead to a better recovery.
Clots busting medication can unblock the blood vessel and improve recovery. However, there is a small risk of complications, most importantly bleeding which may rarely be very severe or fatal.
It may be useful to use written information to support these brief discussions.(see below)
Because Time is brain – it is important not to delay treatment with unnecessarily long discussions about the benefits and risks.
For more detailed information regarding patient and family information see:
Angela is able to communicate, so the medical team talk with her.
After a brief discussion about the benefits and risks Angela agrees to have thrombolysis.
Key point
Identifying goals which can be reviewed after a time limited period will make further discussions about prolonging or withdrawing alternative or clinically assisted nutrition and hydration. This encourages the conversation to be about achieving the patient’s best interests rather than only prolonging life and therefore:
- Confirms the outcome of the trial period of alternative or clinically assisted nutrition and hydration with very little evidence of benefit
- Acknowledges the consistent message from his wife about the patient’s known preferences
- Supports the whole team and allow them to express concerns about withdrawing alternative of clinically assisted nutrition and hydration balancing that with the risks of establishing longer-term alternative or clinically assisted nutrition and hydration
- Highlights the need for caution in discussions with family as there are current values differences between wife and daughter that will need to be dealt with sensitively
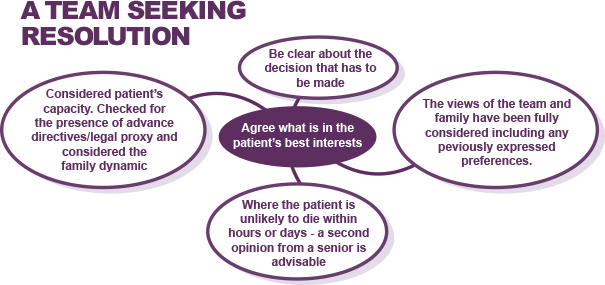
Where there is disagreement between members of the healthcare team about whether clinically assisted nutrition or hydration should be provided, it is important to seek resolution.
Listening carefully and trying to understand each team member’s perspective is important as it provides guidance and facilitates shared decision making. The following table provides some examples of what could be discussed within an MDT meeting and what layers of context can be contained within each statement.
| Things people might say |
Reason for disagreement |
| He’s not had long enough to improve |
Uncertainty of prognosis |
| I would find it very difficult to say |
Personal discomfort with discussion |
| I’d need to ask my senior |
Unsure related to experience |
| We can’t just starve him |
Different values |
| We can’t withdraw a tube now we have started |
Lack of clarity on the legal position |
| I wasn’t aware his family thought that |
Insufficient sharing of information |
Based on the initial assessment, Angela has probably had an acute stroke and is within the time window when thrombolysis (0-4.5 hours) or thrombectomy (0-6 hours) is likely to improve her recovery.
The priority now is to get a non-contrast CT brain scan to exclude a bleed, and to determine whether she has a blocked artery which might be treatable with thrombectomy with a CT angiogram (CTA).
In a patient with a hyperacute stroke the CTA may not only show a blocked artery amenable to thrombectomy but also help determine the cause of the stroke, and even whether later treatment (i.e. after 4.5 hours) with thrombolysis might be effective.
CT angiograms (CTA). Please indicate whether the following statements about CT angiograms are True or False.
It has now been 4 days since admission. Patient remains nil by mouth, minimally responsive, requiring full care and unable to participate in rehab. The multi-disciplinary team discuss again the plan for this patient.
Acknowledge that clinically assisted nutrition and hydration are judged by law to be medical treatments and therefore can be withdrawn if no benefit.
GMC 2010 guidance:
“If there is a reasonable degree of uncertainty about whether a particular treatment will provide overall benefit for a patient who lacks capacity to make a decision, the treatment should be started in order to allow a clearer assessment to be made.”
GMC 2010. Treatment and care towards the end of life: good practice in decision making
The team share their findings from the conversations they have already had with the family
- Daughter wants everything done and concerned about nutrition and hydration
- Wife is still quite shocked and passive in discussions with her daughter taking charge
![Dr Richards reviews the case and considers how to approach the conversation with the family. [See View Text Alternative button for details of text in thought bubble.]](/wp-content/uploads/2020/04/Doc_thought_47564.jpg)
- Hamish McLeod, a 67-year old retired accountant
- Presenting with a left hemisphere TACS
- Previous stroke and wheelchair bound. Reports of depression post stroke
- Lives with a wife who is in good health
- He has 2 grown-up daughters both of whom are very involved and supporting their mother regularly on hospital visits
Key Points
The overall approach to care should be agreed by shared decision-making based on the expected prognosis for the patient.
Conversations about nutrition and hydration can take place both formally and informally with different members of the multi-disciplinary team. Treatment decisions are very likely to change over time and it is important that families do not feel they are receiving conflicting information.
This section will look at a sequence of discussions between a patient’s family and the multidisciplinary team focussing on:
- Initial explanations to a family that there is a problem with swallowing and consider how to address their initial questions and concerns about treatment plans
- Initial team discussions about nasogastric (NG) feeding which reveals some uncertainty between members but a shared desire for a clear decision on whether active or supportive care is appropriate
- Team assessment of the perceived benefits from a trial of alternative nutrition and hydration or clinically assisted nutrition and hydration and considering how to deal with potential disagreements on future treatment plans
- Discussion with family which reveals conflict in opinion between family members about the risks and benefits of alternative nutrition and hydration or clinically assisted nutrition and hydration
- Responding to concerns expressed about hunger/thirst/choking
- Support to the family and nursing team on how to approach eating and drinking for comfort and good oral care

Introduction
The RCP have recently updated their guidance document for supporting people who have eating and drinking difficulties, particularly at end of life, which aims “to guide an approach to finding a way through these difficulties that is legally sound, pragmatic and compassionate”. “The difficulties, uncertainties and confusion associated with decisions regarding provision of nutrition and hydration towards the end of life remain extremely challenging”. “In most cases there are no easy answers but rather approaches to follow to reach the best decision for each individual patient” (RCP, 2021).
RCP Report of a working party, Supporting people with eating and drinking difficulties. March 2021. Link to RCP report.
- Decisions about nutrition and hydration can cause dilemmas and differences of opinions between professionals and families. Everyone understands that receiving nutrition and hydration is essential to life and therefore failure to adequately address and explain the issue can result in lack of nutrition and hydration being blamed for the person’s deterioration
- Decisions about nutrition and hydration often run in parallel with decisions on overall prognosis and therefore may change and risk giving mixed messages if there is poor communication within the team and with the family
- Discussions need to take account of previous explanations given and attempt to understand the perspectives of the people involved
- Families and the healthcare team will require practical advice and support to manage oral care and provision of food and fluid at the end of life
Disclaimer: Within this section of the module, there are a number of infographics which include the now outdated term “feeding”. Out with these infographics we have updated terminology to avoid the use of “feeding”, this includes nutrition and hydration, assisting with eating and drinking and eating and drinking with acknowledged risks. The RCP (2021) report preference for “eating and drinking” over “oral feeding”, with aim of moving towards a more person-centered approach. The Royal College of Speech and Language Therapists (RCSLT, 2021) encourage the use of the term “eating and drinking with acknowledged risks” versus “risk feeding” or similar terms.

![Dr Richards reviews the case and considers how to approach the conversation with the family. [See View Text Alternative button for details of text in thought bubble.]](/wp-content/uploads/2020/04/Doc_thought_47564.jpg)



