What questions should you ask Vince and Nigel?
Specific to their problems
- Are you having any problems with your vision?
- Do you feel your vision has altered? In what way?
- Have you had double vision, where you see two of something?
- Specifically, do you have difficulties with TV, reading or bumping into things?
- How long have you noticed the changes for?
More general questions about their vision
- Do you have any glasses? When was your last eye test? Who is your optician?
- Do you drive?
- Do you have any previous eye problems that you know of? For example, glaucoma, cataract?
- Have you had any eye problems before your stroke?
- Have you been seeing anything that might not / should not be there? Maybe patterns, faces or people?
Visual hallucinations may occur following significant visual loss. Patients rarely volunteer these symptoms and it is therefore important to ask if they are present. This condition is called Charles Bonnet Syndrome and the following information leaflet may assist your learning and be useful to stroke survivors: Stroke Charles Bonnet leaflet [PDF, 27K] (with permission of the British & Irish Orthoptic Society)
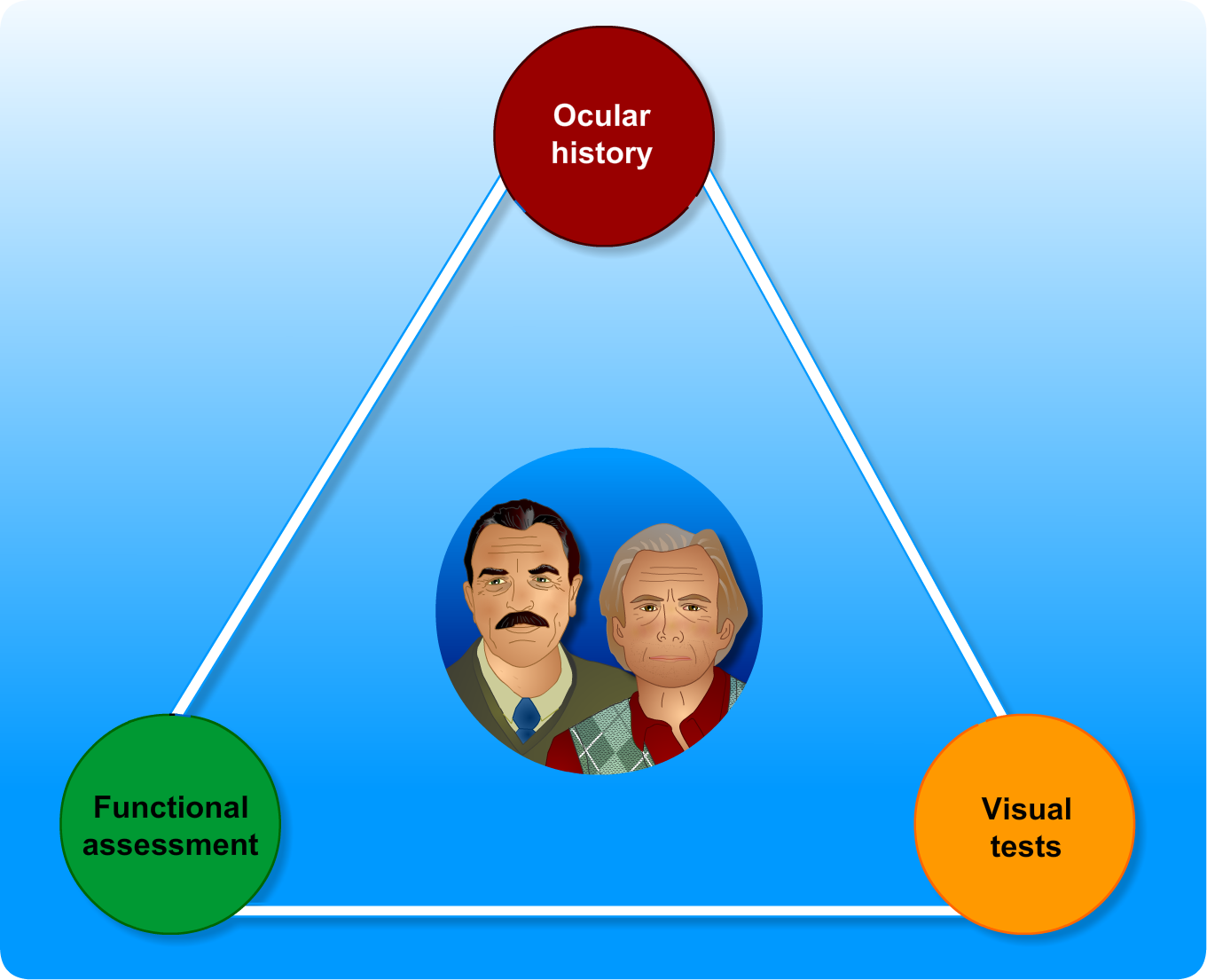
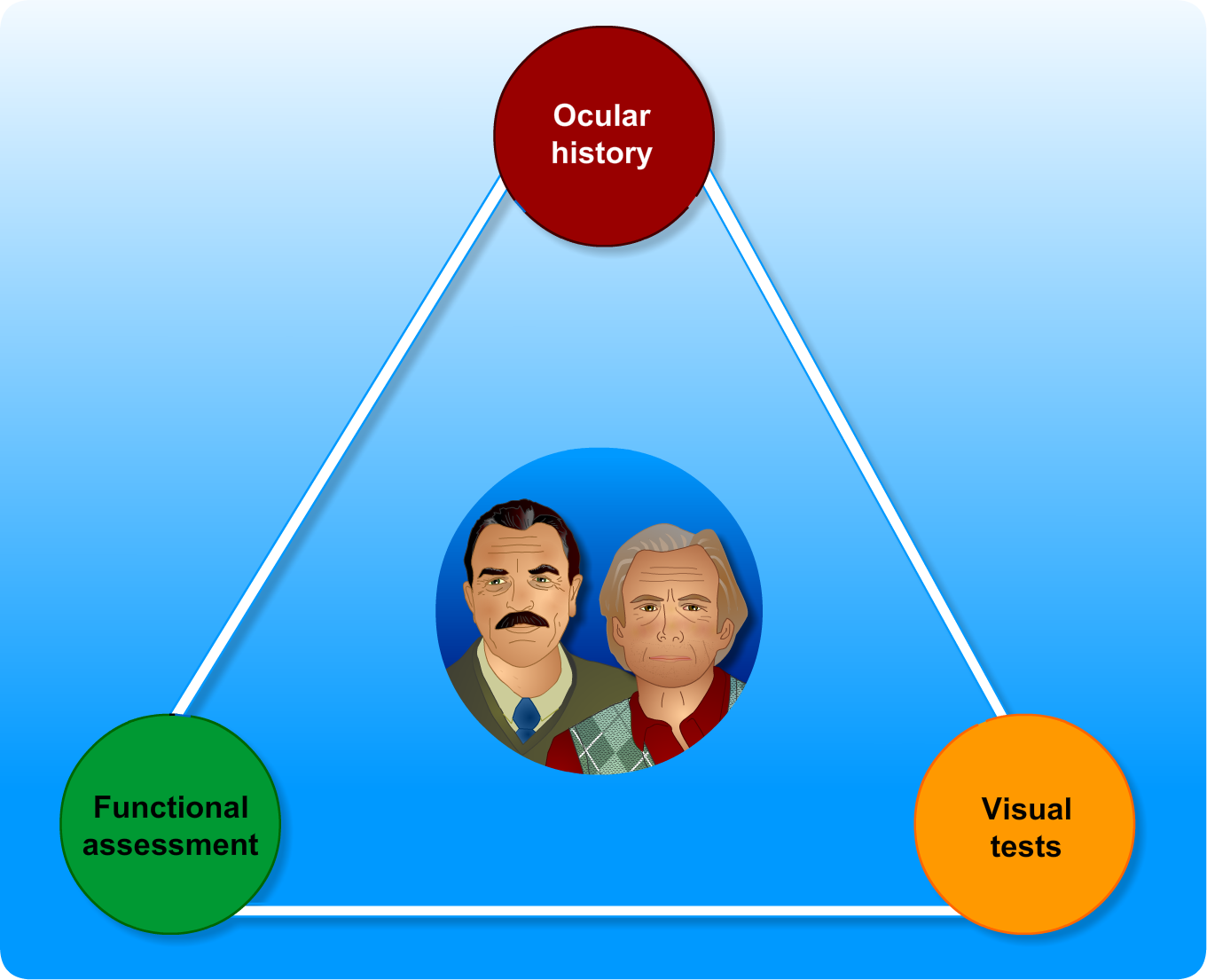
The MDT decide that Vince and Nigel should both undergo a visual screen. Visual screening should include an ocular history, visual tests and a functional assessment. Click on the links below the diagram for further information.
A number of visual screening tools are available – you may wish to use one of the tools listed below. These can be utilised by any appropriately trained staff to allow accurate assessment and to inform patient management. If staff need training in how to perform visual screening, they may wish to speak to the local eye department, to see if they can conduct training.
Paper-based screening tool.
VISA screening tool
app, via the Apple store: apps.apple.com/gb/app/visa-screen/
The ‘Heart Disease and Stroke Action Plan’ published in June 2009 identified the need to provide specialist training for nurses and to increase the range of opportunities for all staff to gain the knowledge and skills required in stroke care.
This e-learning resource provides a set of ‘Advancing Modules’ which builds on the core knowledge and skills covered by the Stroke Core Competencies.
Please consider images and text size may vary depending on your screen device and settings. Also, to be able to successfully complete module assessment(s) some information may be contained within ‘Interactive Quizzes’, ‘Additional Information’ or associated ‘Topic Loops’.
Latest News:
January 2024: Chest Heart & Stroke Scotland, in collaboration with professional experts in stroke care across Scotland, are delighted to announce the launch of the updated STARs eLearning advancing module 6: Cognition following stroke. This resource follows on from the recently updated STARs core competency module 16: Thinking processes and behaviour where some of the people we meet within STARS core competency16 are followed up in STARS AM 6 so we recommend that you complete STARS core competency 16 before starting STARS advancing module 6.
Details of CHSS General Medical Disclaimer can be viewed at the bottom of the page.
 On completion of this module you should now have a critical understanding of the common physical complications which can occur following stroke and how these may be prevented. Where complications have arisen you should understand the importance of early detection and appropriate management.
On completion of this module you should now have a critical understanding of the common physical complications which can occur following stroke and how these may be prevented. Where complications have arisen you should understand the importance of early detection and appropriate management.
You will have learned:
- Which important common physical complications can occur following stroke
- How to recognise the clinical features of those common physical complications
- Strategies to prevent the development of common physical complications
- Individual assessment and treatment strategies for particular physical complications
- About establishing a regimen for maintaining a patient’s optimal physical condition to promote recovery
- The benefits of prompt interventions on patient outcomes with respect to physical complications
The following common physical complications have been covered in this module:
- Hemiplegic shoulder pain
- Abnormal muscle tone
- Chest infection
- Pressure ulceration
- Deep vein thrombosis
- Limb swelling (oedema)
Consider disimpaction regime with macrogol e.g. Movicol™, Laxido™ (as recommended in British National Formulary) following discussion with multi-disciplinary team.
If the above felt to be inappropriate or is unsuccessful consider:
- If stool in rectum, consider suppositories or enema regime
- If rectum empty, consider oral softener and/or stimulant laxative
- A combination of oral and rectal medication
[link to Post gastrostomy insertion and management of gastrostomy tube/site]
- Your visual field is the visual information that is seen (both centrally and peripherally) when you look straight ahead.
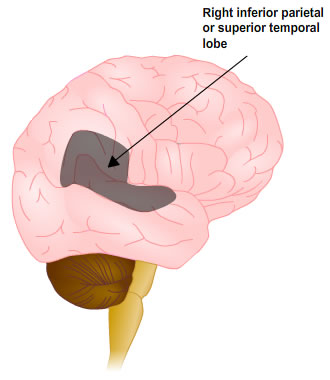
- Visual field loss that occurs following a stroke commonly affects the vision of both eyes and the area of sight loss is always contra-lateral to the stroke location.
- It occurs equally often in right and left hemisphere strokes.
- Visual field loss can be one of the presenting symptoms of stroke, often described by the person as blurred or obscured vision. People may complain of visual field loss in one eye and explain that their vision ‘is not right’.
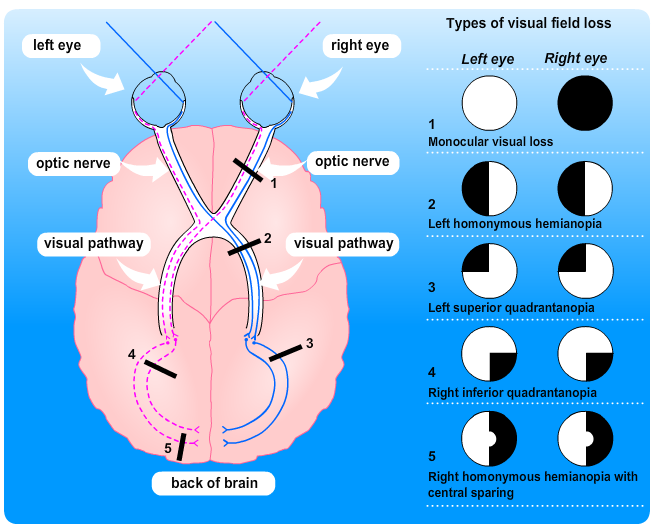
Visual field loss can occur in many different forms and the diagram below illustrates the visual pathway and the potential defects. A stroke that causes visual field loss can affect the pathway at 2, 3, 4 or 5. Strokes that only affect the visual fields most commonly affect the occipital lobe – position 5. Strokes which cause a combination of problems such as unilateral limb weakness, speech problems AND visual field loss more often affect positions 2, 3 and 4. Although not classified as strokes (because they don’t affect the brain itself) ischaemic lesions in the optic nerve (position 1) or retina can lead to loss of vision in one eye only. Traditionally, transient loss of vision in one eye due to an ischaemic lesion is referred to as amaurosis fugax and is classified rather confusingly as a TIA.
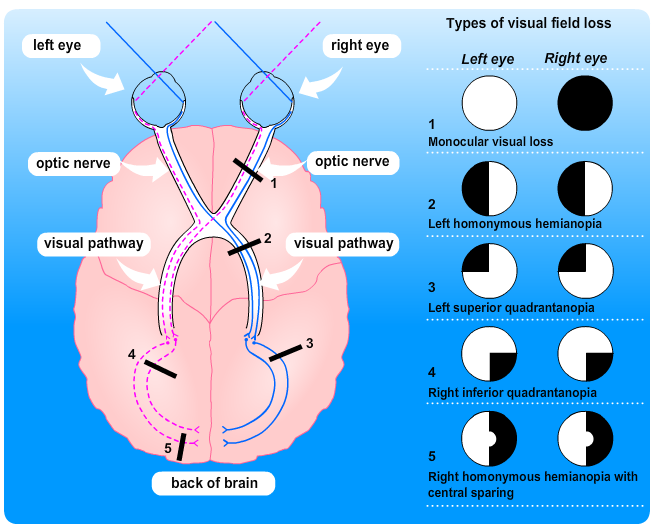
For a short explanation of each of the types of visual field loss illustrated in the drawing above, see the Additional Information box below.
As you will have seen from the hierarchy of vision shown in the module introduction (see Additional Information box to view this again), visual fields form part of the base of the pyramid. They provide us with full and clear visual information upon which the higher levels of visual processing depend.
For more information about screening, assessment and management of vision problems in the first 30 days after an acute stroke see the following best practice statement: Best Practice Statement for Screening, Assessment and Management of Vision Problems in the First 30 Days after an Acute Stroke
 Visual neglect and inattention are also referred to as hemiagnosia, hemineglect, unilateral neglect, spatial neglect, unilateral visual inattention, hemi-inattention or neglect syndrome.
Visual neglect and inattention are also referred to as hemiagnosia, hemineglect, unilateral neglect, spatial neglect, unilateral visual inattention, hemi-inattention or neglect syndrome.
 On completion of this module you should now have a critical understanding of the common physical complications which can occur following stroke and how these may be prevented. Where complications have arisen you should understand the importance of early detection and appropriate management.
On completion of this module you should now have a critical understanding of the common physical complications which can occur following stroke and how these may be prevented. Where complications have arisen you should understand the importance of early detection and appropriate management.