Katie attends the paediatric cardiology clinic for assessment, where it is diagnosed that her unborn baby has severe Tetralogy of Fallot (ToF). The condition is explained to the parents, prior to Katie meeting with the consultant obstetrician to discuss the implications of this for her pregnancy.
What is Tetralogy of Fallot?
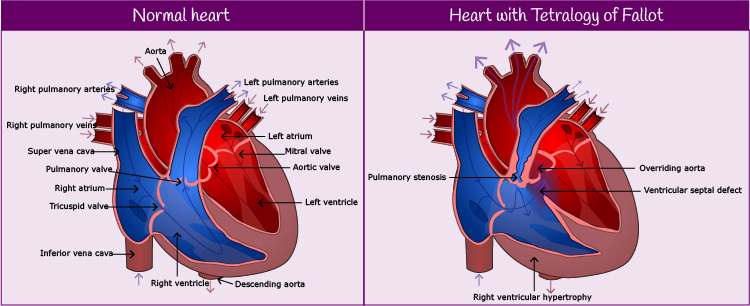
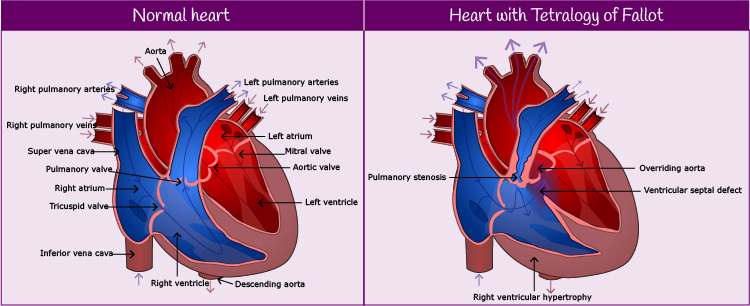
ToF is one of the most common forms of cyanotic congenital heart disease and requires surgical intervention once the baby is born. ToF is made up of four features:
- a ventricular septal defect
- an overriding aorta (taken with a ventricular septal defect, this causes oxygenated and non-oxygenated blood to mix)
- pulmonary stenosis
- right ventricular hypertrophy (results from the pulmonary stenosis)

Kirsten: pre-natal
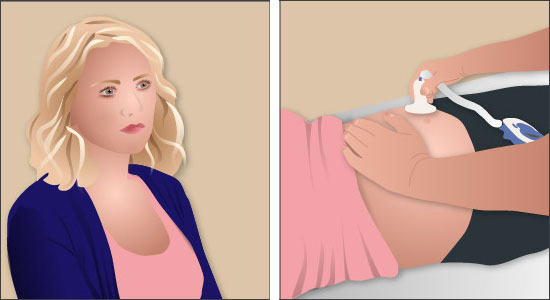
Katie is 18 weeks pregnant with her first baby and attends the ante-natal clinic for a routine anomaly scan. During the scan, the midwife sonographer notices abnormalities in the baby’s heart.
The sonographer asks the consultant obstetrician to review the scan results and a repeat scan is performed. Agreeing that the scans indicate the presence of heart defects, the obstetrician refers the baby to a foetal cardiologist.
Please enable JavaScript in your browser to see this interactive content.

Following his surgery as a baby, Jack goes on to lead a normal life. He loves football and plays regularly for his school team. He continues to attend the cardiology clinic for review until he is discharged at the age of sixteen.
Please enable JavaScript in your browser to see this interactive content.
Pulse point
There are a number of causes of congenital heart defects. One of these is rubella which, although it is not a serious infection for adult, can have a very serious effect on an unborn baby if a mother develops rubella in the first 8-10 weeks of pregnancy. Rubella vaccine is now offered as part of the routine childhood vaccination schedule.
Jack has an echocardiogram performed. The investigation shows that Jack has a ventricular-septal defect. This is a hole in the wall that separates the right and left ventricles of the heart. It is one of the most common congenital heart defects.
Please enable JavaScript in your browser to see this interactive content.
Based on the results of the echocardiogram, the cardiologist concludes that Jack will require surgery to repair the hole in his cardiac septum.
Please enable JavaScript in your browser to see this interactive content.
Jack and his parents attend hospital for an appointment with a cardiologist. The cardiologist examines Jack and suggests to the parents that Jack should have an echocardiogram performed.
Please enable JavaScript in your browser to see this interactive content.
The cardiologist arranges for Jack to have an echocardiogram performed in the department that day.
When Jack is three weeks old, the health visitor pops in for a routine visit. Jack’s mum is worried that he is not thriving as well as some of the other babies of the same age that she sees at her local breast-feeding support group and shares her concerns with the health visitor.
Please enable JavaScript in your browser to see this interactive content.
Jack appears to be breathless and, as a consequence, is not feeding well. The health visitor weighs and measures Jack and finds that Jack is underweight and small for his age.
She is concerned about Jack and arranges for him to have an appointment with the GP later that day. Having examined Jack, the GP shares the health visitor’s concerns and suspects that Jack may have a cardiac condition. He refers him to a cardiologist for urgent assessment.

Jack’s Story

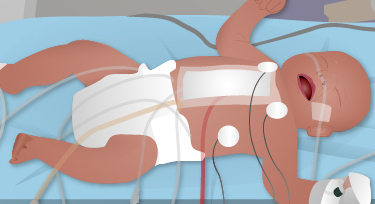
Meet Jack. His mother, a first time mum, gave birth to him two days ago, after an uneventful pregnancy and a normal delivery. Routine assessments of Jack were satisfactory and he and his mum were discharged home, into the care of the community midwives.

Andrew is coping well with his condition. He continues to attend regular reviews at the cardiology and ICD clinic, where he is monitored for the presence of atrial fibrillation and any signs of heart failure.
HCM is a life-long condition and, now that he has been diagnosed, Andrew has to think about the implications of this for his future lifestyle.
Andrew, the arrythmia nurse and the school nurse draw up a Care Plan, which outlines Andrew’s condition and treatment.
| Hypertrophic Cardiomyopathy / School Care Plan Template |
| Child’s name: |
Andrew |
DOB: |
21/03/2000 |
| School: |
Dundee Academy |
| Diagnosis: |
Hypertrophic Cardiomyopathy (HCM) |
| Procedures: |
Subcutaneous – Implantable Cardiac Defibrillator (S-ICD) |
| Condition: |
HCM is a disease resulting in excessive thickening (hypertrophy) of the hearts muscle. This condition is progressive and thickening of the muscle can become worse over time resulting in the development of symptoms.
HCM may affect the way in which the heart muscle pumps; the heart muscle becomes weak and ineffective at pumping blood around the body. As the heart muscle thickens this can also cause obstruction of blood flow so that too little blood is pumped out of the heart and around the body.
HCM also predisposes to changes in the heart’s rhythm which may lead to collapse, loss of consciousness and sudden cardiac death. |
| Potential Symptoms: |
- Fainting
- Dizziness
- Risk of rapid/irregular heart beat (palpitations)
- Rapid breathing rate/Shortness of breath
- Fatigue
- Irritability
- Chest pain
- Poor exercise tolerance
- Sudden cardiac arrest
|
| Medications: |
Should changes in the heart rhythm occur medications are taken to control the heart rhythm and reduce the risk of collapse occurring. Andrew is taking medications to control his heart rhythm. This slows his heart rate and prevents changes that could precipitate fainting or the above mentioned symptoms. This medication is called Bisoprolol. Andrew also takes Ramipril to improve his heart function. |
| Daily Activities: |
Andrew should participate in gentle sporting activities and should be allowed to self limit and sit out when needed.
Andrew should also avoid competitive/highly intense physical exercise and contact sports. It has been agreed that he can play football for leisure purposes but not at a competitive level.
Andrew should attend school as normal and should be encouraged to fulfil his potential. He should be treated as normally as possible.
Andrew will also need time off school to attend outpatient appointments. |
| Emergency Treatment: |
- In the event of collapse and loss of consciousness please dial 999.
- Basic life support (BLS) should be commenced and continued until paramedics arrive or until consciousness regains.
- Andrew has an internal cardiac defibrillator that will fire internally if his heart rhythm requires this. An internal shock will not affect the rescuer if this occurs during BLS.
|