Jimmy and his wife arrive at the Emergency Department of the thrombectomy hub. There is a local protocol for the management of patient’s arriving with a suspected stroke which should be followed. Protocols provide a clear written description of appropriate action required under specific circumstances.
- Taken into area defined locally for hyperacute assessments (perhaps Resus in ED, or a specific bay, or in some hospitals into the scanning dept
- Met by doctor and nurse
- Rapid assessment to confirm diagnosis of probable stroke – determine deficits with the National Institutes of Health Stroke Scale (NIHSS) – all medical and nursing staff involved in hyperacute stroke care should complete training in this
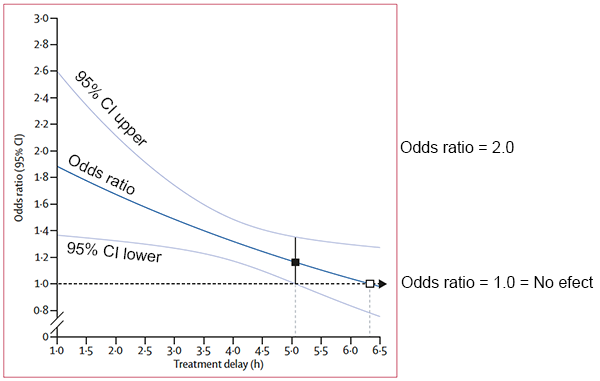
- Assess for eligibility for thrombolysis and thrombectomy (onset time, severity warrants hyperacute treatment)
- Insert iv cannula to allow injection of contrast for CTA, and administration of thrombolysis if appropriate
- Arrange immediate CT and CTA (if eligible for both thrombolysis and thrombectomy)
- If imaging ready take patient through, don’t wait for porters!