Aims of treatment

Images subject to copyright. Anatomical diagrams are reproduced with permission from Jost, W; Pictorial Atlas of Botulinum Toxin Injection: Localization, Application; Quintessence Publishing Co Ltd; August 2008. Courtesy of Merz Pharma UK. M-MP-UKI-0059.
The primary aim of the treatment of hypertonus or spasticity in muscles is:
- to maintain length
- to allow normal positioning of the limbs
This will help prevent secondary soft tissue shortening.
“The mainstay of treatment is muscle stretching, and splinting/orthotics provide a means to maintain prolonged stretching in between sessions of physiotherapy and manual handling” (Verplancke et al 2005).
The primary aim of the treatment of hypotonus or flaccidity in muscle is:
- to preserve alignment of muscle and joints
- to preserve function
Any intervention should be aimed at facilitating these fundamental treatments. This role should be multidisciplinary and part of the patient’s everyday treatment and care planning.
Irene is an 84-year old lady who is a resident of the Sunrise Nursing Home. Judith is 82 years old and is in the room next to Irene. Both ladies had a stroke in the same week one year ago, which resulted in them experiencing left weakness and neglect. Their left arms developed spasticity. A core part of managing this was daily stretches by the therapy and nursing staff to make sure they had the opportunity for their arms and legs to be moved through their full range of motion. Despite the best efforts of the stroke acute and rehabilitation units, neither lady achieved adequate independence to return home and, after eight months, found places in Sunrise.
Sunrise Nursing Home is a modern and well-run nursing home. The staff are trained well and the environment is clean and well-maintained. However, its popularity has led to it operating consistently at nearly full capacity. The staff are always busy and they are limited to providing this additional care routine for the residents.
Irene’s two sons, their wives and various grown-up grandchildren visit her regularly. They were taught by the therapists in the hospital how to stretch Irene’s arm, hand and leg and they do this whenever they visit. In contrast, Judith’s family live 400 miles away and they can only visit occasionally and were never taught how to stretch Judith’s arm and leg. The Sunrise staff do not have the time to provide the stretching that Judith needs.
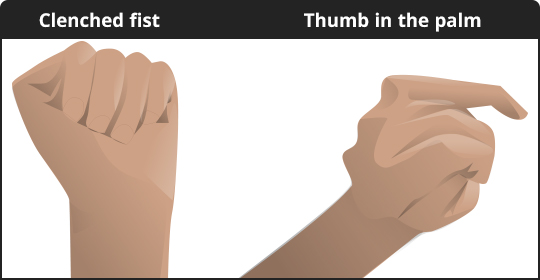
Although, Irene’s left elbow and hand can become tight, she is able to straighten them by using her right hand and she remains comfortable. Sadly, Judith’s elbow and fingers can no longer be fully stretched out as her muscles have permanently shortened due to the lack of stretching. She has developed muscle contractures. The staff of Sunrise must keep swabs in her left hand as the tightness is now causing her fingernails to dig into the palm of her hand.
The story of Irene and Judith emphasises how important it is for people to have the opportunity for their limbs to be moved through their full range of motion on a daily basis.
- When a muscle becomes shorter it becomes stiffer, less easy to move.
- Re-lengthening occurs by creep.
- Creep allows soft tissues to tolerate applied loads by lengthening, but only occurs at end of range/when stretched out of position.
- As a muscle lengthens it regains sarcomeres plus tension and therefore the ability to contract.
As overall volume of sarcomeres increases, there is a relative reduction in the amount of connective tissue present which makes the muscle less stiff and more elastic – so less resistant to passive stretch.
There are three types of skeletal muscle fibres.
- Slow oxidative – these contract relatively slowly and use aerobic respiration (oxygen and glucose).
- Fast oxidative – have faster contractions but because they may switch to anerobic respiration (gycolysis) they can fatigue more quickly than slow oxidative fibres.
- Fast glyolytic fibres – faster contraction using primarily anerobic glycolysis. These fibres fatigue more quickly than the other fibres.
Changes in muscle fibre properties i.e atrophy, result in an increase in number of fast oxidative fibres and decrease in slow oxidative fibres – this can also be reversed.
Ability to generate tension is best at optimum length – so muscle is able to contract and function as needed.
‘Stretching normal muscle leads to mechanical changes in shape through creep’
(Gelinas et al, 2000)
Creep
A progressive deformation when a constant load is applied over time; it allows soft tissues to tolerate applied loads by lengthening.
- Holding the stretch for a length of time, repeatedly, leads to permanent lengthening of muscle.
- We know that repeated stretching for long enough to allow tissue lengthening, leads to change in the physical structure of the muscle. However we don’t know what the optimum time is to get the best effect.
- Recommended time varies from 30 mins (Tardieu et al, 1988) to 6 hours (Williams, 1989).
- We also need to consider the effect on the opposing muscle groups. Muscle groups work by allowing opposite movements when one group is active the other is relaxed – e.g. if you stretch hamstrings for prolonged periods you are effectively exposing quads to the effects of immobility in a shortened position.
The Tardieu study found that after 30 mins stretching, sarcomeres got longer and more in number. This increase in number was greater with a stretch of 2 hours. The treatment time must be realistic so you must consider if it is achievable in the setting be it hospital or home.
Guissard et al, 2004, found in healthy subjects, that passive stretching (10 minutes of stretching a day for 30 days over 6 weeks) can reduce the tendon’s sensitivity to stretch.
The Williams study looked at prevention of soleus contracture and found that to prevent soleus shortening in individuals with stroke and spasticity, the muscle had to be in a lengthened position for 6 hours per day – is this achievable in hospital or community setting? It certainly is a lot to ask any individual to take out of their day. It also may not be applicable to many of our patients or clients. However stretching remains important and regular stretching should be part of the patients treatment plan for reducing spasticity and to protect movement of joints.
Goals of the treatment are important- if your patient is aiming for weight bearing, gait or transferring in standing on to walking then it matters a lot. If your patient is aiming to be able to sit in a wheelchair and is hoist transferred then it may not be as important for function but could lead to complications from contractures including pain and tendon shortening. Remember to ask what the patient’s self-management goals are in relation to movement and lifestyle.
Contracture
“Is the chronic loss of joint motion due to structural changes in non-bony tissues including muscles, ligaments and tendons”
The Free Dictionary: Medical Dictionary: Contractures
or
“A condition of shortening and hardening of muscles, tendons or other tissue, often leading to deformity and rigidity of joints”
English Oxford Dictionaries: Contracture
Why do contractures develop?
Any joint not moved through its normal range of motion will develop a contracture.
Main factors leading to contractures after stroke are:
- Immobilisation or immobility.
- Spasticity.
- Muscle weakness and paralysis.
Spasticity does not directly cause muscle contracture, however it does predispose a person resting with muscles in a shortened position.
Relevance for practice
Patients who spend prolonged periods of time with muscles in shortened positions e.g. sitting in a chair all day shortens hip and knee flexors, weakness of the upper limb leads to people sitting with their arms in internal rotation with flexion and pronation.
There also seem to be some people with a predisposition to tendon shortening.
The following good practice principles can help to minimise the negative effects of spasticity:
- MDT assessment and goal planning to include spasticity management.
- Identify and treat any aggravating factors.
- Ensure there is an appropriate 24-hour postural management programme which includes positioning, stretching, splinting if necessary, self-management, carer involvement.
- Ensure there is an appropriate programme of physical therapy and activity.
Key points
- Spasticity should not result in contracture, although spasticity predisposes a person to resting with muscles in a shortened position.
- Immobilisation in a shortened position is what causes contracture.
The video will pause at important points, press play to continue.
Following a stroke, patients may present with abnormal muscle tone which will interfere with movement. It may be decreased which can be referred to as Flaccidity (Hypotonus), increased which can be referred to as Spasticity (Hypertonus) or a combination of the two. A combination of the two occurs where there is increased tone in one muscle group and decreased tone in another.
Tone may be increased temporarily by pain, discomfort, anxiety, effort and certain body positions.
Here are some simple clinical signs to differentiate low tone (Hypotonus) from high tone (Hypertonus):
- Hypotonus: Low toned muscles are floppy and sag away from their bony connections leaving the associated joints unsupported and unstable. Low toned limbs feel heavy and drop against gravity when handled if insufficient support is given. The muscle groups will feel flabby to handle and little or no resistance will be felt through the range of the movement. Great care must be taken to ensure adequate support of joints throughout their range of movement to prevent trauma injuries, particularly to the shoulder.
- Hypertonus: High toned muscles are tense and bulky, with tendons visible beneath the skin. Joints which are spanned by high tone muscles will assume a shortened position rendering the patient unable to relax. High toned muscles will resist movement and feel tight.
Stroke affects the mechanism which controls the resting levels of muscle activity. There are 2 components to hypertonia:
- Neurological
- Non neurological (musculoskeletal)
Spasticity and hypertonia are not interchangeable terms but principles for treatment are similar.
Now you try to assess four patients using the FAST test. Watch the videos and answer each of the questions superimposed on the video.
The videos below are provided by kind permission: Mark Garside – Northumbria Healthcare; Chris Price – Newcastle University.
Patient 1
Duration: 34 seconds
Patient 2
Duration: 28 seconds
Patient 3
Duration: 47 seconds
Patient 4
Duration: 33 seconds
Clonus
“The repetitive movement or ‘jumping’ caused by the alternate stretching and unloading of the muscle spindles”… as a reaction to stretch e.g. foot on foot plate triggering stretch reflex due to shortened plantarflexors – “rhythmic contractions of both gastroc and soleus in response to dorsiflexion of the ankle”
Stevenson VL, Spasticity Management, Clinical Rehabilitation 24: 293-304, 2010
“Alternate involuntary muscle contraction in rapid succession which can be set in motion by reflex testing.”
clonus. (n.d.) Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. (2003). Retrieved September 12 2017 The Free Dictionary: Medical Dictionary
Spasms
Sudden involuntary movement frequently “precipitated by muscle stretch, they can also be triggered via a variety of peripheral, noxious and visceral afferents e.g. pressure sores, bowel impaction, urinary retention or infection”
Stevenson VL, Spasticity Management, Clinical Rehabilitation 24: 293-304, 2010
Fasciculation
Small involuntary muscular contractions visible under the skin.
Myoclonic jerks
Short lived motor twitches of isolated, involuntary movement.
“Spasticity is a motor disorder characterised by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon reflexes, resulting from hyper-excitability of the stretch reflex, as one component of the upper motor neurone syndrome”
Lance J. Spasticity: disorders motor control. In: Feldman RG, Young RP, Koella WP editors. Symposium synopsis. Miami, FL: Year Book Medical Publishers; 1980.
Lance’s definition does not include other features of the upper motor neurone syndrome such as spasm and clonus.
Alternative definition:
“Disordered sensorimotor control, resulting from an upper motor neurone lesion, presenting as intermittent or sustained involuntary activation of muscles”
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, Hermens H, Johnson GR. 2005. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil, vol. 27(1-2), 2-6
“In spasticity an enhanced and prolonged response to muscle stretch is seen at rest” – hyperexcitable – with a decrease in inhibitory spinal cord control
Stevenson VL, Spasticity Management, Clinical Rehabilitation 24: 293-304, 2010